WHAT IS RADIOFREQUENCY ABLATION OF LIVER TUMOURS?
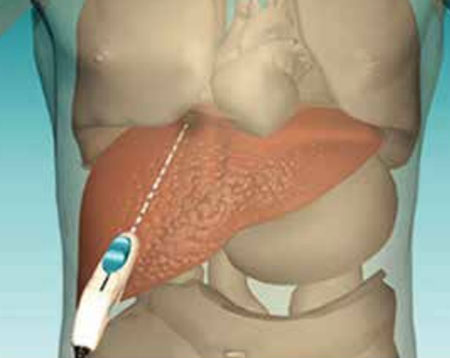
Radiofrequency ablation (RFA) is a minimally invasive, repeatable procedure with few complications used to treat small, often inoperable, metastatic (particularly from colon cancer) and primary (hepatocellular carcinoma) tumours of the liver.
Percutaneous RFA is an effective treatment option for patients who might have difficulty with surgery or those whose tumours are less than 3.5 cm in diameter. It may be used in addition to chemotherapy, radiation therapy or surgery or as an alternative surgical treatment. The success rate for completely eliminating small liver tumours is greater than 85 per cent.
Percutaneous RFA uses imaging guidance such as ultrasound or computed tomography (CT) to place a needle electrode through the skin into a liver tumour. High-frequency electrical currents are passed through the electrode, creating heat that destroys the cancer cells. At the same time, heat from radiofrequency energy closes small blood vessels and lessens the risk of bleeding. The dead tumour cells are gradually replaced by scar tissue that shrinks over time.

RFA can also be performed during open or laparoscopic surgery as in some cases superficial tumours can be wedged out (excised) surgically, while deeper lesions can be destroyed by RFA, thereby preserving most of the liver tissue.
INDICATIONS
The range of indications for percutaneous RFA is becoming wider and includes the following main categories:
- Hepatocellular carcinoma at an early stage
- Primary treatment for small tumors
- Inoperable primary liver tumor
- Treatment of patients who cannot undergo general anesthesia or are not operative candidates because of comorbidity or advanced age
- Liver metastasis, most commonly from colorectal cancer, especially if the patient is not an operative candidate
- Can be used for breast, thyroid, and neuroendocrine cancers metastasis
- Treatment of patients who have a single hepatocellular carcinoma or multiple small lesions and are waiting for liver transplantation
- Recurrent and progressive lesions
RFA is a relatively quick procedure and recovery is rapid so that chemotherapy may be resumed almost immediately in patients who need it.
HOW SHOULD I PREPARE?
You may be instructed not to eat or drink for eight hours before your RFA.
Prior to a RFA, you should report to your doctor all medications that you are taking, and if you have any allergies, especially to anaesthesia or to contrast media containing iodine. Also, inform your doctor about recent illnesses or other medical conditions. Women should always inform their doctor if there is any possibility that they are pregnant.
Your doctor will advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners three days or more (depending on the drug) before your procedure. Prior to your procedure, your blood coagulation may be tested.
WHAT DOES THE EQUIPMENT LOOK LIKE?
The equipment used in this procedure depends on the type of imaging guidance.
The radiofrequency generator produces electrical currents in the range of radiofrequency waves. It is connected by insulated wires to the needle electrodes and to grounding pads that are placed on the patient’s thigh.
Other equipment that may be used during the procedure includes an intravenous line and devices that monitor your heart beat and blood pressure.
HOW IS THE PROCEDURE PERFORMED?
Image-guided, minimally invasive procedures such as RFA are most often performed by a specially trained interventional radiologist in the operating room or in the Imaging Department.
RFA is usually done on an inpatient basis. You are usually hospitalised the day before the procedure and discharged on the next morning.
During the procedure:
- You will be positioned on the examining table.
- You may be connected to monitors that track your heart rate, blood pressure and pulse during the procedure.
- A nurse will insert an intravenous line into a vein in your hand or arm so that sedation medication can be given intravenously.
- The area where the electrodes are to be inserted will be sterilized and covered with a surgical drape.
- Your doctor will numb the area with a local anaesthetic. A very small nick may be made in your skin to make it easier to pass the RFA electrode into your liver.
- Using imaging-guidance, your doctor will insert the needle electrode through the skin and advance it to the site of the tumour.
- Once the needle electrode is in place and your sedation effective, radiofrequency energy is applied. For a large tumour, it may be necessary to place multiple needles. At the end of the procedure, the needle electrode will be removed and will coagulate tissues on its way. The opening in the skin is covered with a dressing.
Each RFA takes about 30 minutes, with additional time required if multiple ablations are performed. The entire procedure is usually completed within one to two hours.
WHAT WILL I EXPERIENCE DURING AND AFTER THE PROCEDURE?
You will feel a slight pin prick when the needle is inserted into your vein for the intravenous line and when the local anaesthetic is injected. Most of the sensation is at the skin incision site which is numbed using local anaesthetic.
If the case is done with sedation, the intravenous sedative will make you feel relaxed and sleepy. You may or may not remain awake, depending on how deeply you are sedated. If you are put under general anaesthesia, your throat may be sore after you wake up. This is caused by the breathing tube that was placed in your throat while you were asleep.
Pain immediately following radiofrequency ablation can be controlled by pain medication given through your intravenous line or by injection. Afterward any mild discomfort you experience can be controlled by oral pain medications. Patients may feel nauseous, but this can also be relieved by medication.
You will remain in the recovery room until you are completely awake and ready to return to your room.
You should be able to resume your usual activities within a few days.
Only about ten percent of patients will still have pain a week following radiofrequency ablation
WHO INTERPRETS THE RESULTS AND HOW DO I GET THEM?
Computed tomography (CT) or magnetic resonance imaging (MRI) of the liver is performed within a few days to a month following radiofrequency ablation. A radiologist will interpret these CT or MRI scans to detect any complications and to ensure that all of the tumour tissue has been destroyed.
You will undergo CT or MRI scans every three to four months to check for new tumours.
WHAT ARE THE RISKS OF THE PROCEDURE?
- RFA is a safe procedure with very low rates of death and major complications and is generally well-tolerated with minimal to no pain after the treatment. Severe pain after RFA is uncommon, but may last a few days and require a narcotic to provide relief.
- Some people will experience a low-grade fever for a few days after the procedure.
- There is a very low risk of bleeding or infection after the treatment.
- Depending on the site of treatment, radiofrequency ablation may cause brief or, rarely, long-lasting shoulder pain; inflammation of the gallbladder that subsides after a few weeks; damage to the bile ducts resulting in biliary obstruction; thermal damage to the bowel; or pleural effusion.
- Some patients may develop a “post-ablation syndrome” with flu-like symptoms that appear three to five days after the procedure and usually last about five days. An occasional patient may remain ill for two to three weeks. Acetaminophen or ibuprofen taken by mouth is commonly used to control fever and other symptoms.
- Organs and tissues near the liver, such as the gallbladder, bile ducts, diaphragm and bowel loops, are at risk of being injured. Although this occurs only 3 to 5 per cent of the time, it may require surgical correction. The risk of this complication is related to the location of the liver tumour that is treated.
WHAT ARE THE LIMITATIONS OF RADIOFREQUENCY ABLATION OF LIVER TUMOURS?
There is a limit to the volume of tumour tissue that can be eliminated by RFA. This is due to limitations with current equipment. Hopefully technical advances will permit larger tumours to be treated in the future. RFA also cannot destroy microscopic-sized tumours and cannot prevent cancer from growing back in other locations in the liver.

 Vi
Vi