Some people are prone to stones forming in the kidney. Some of these do not give you any problems while others, if left untreated may grow and cause damage to the kidneys. Urine is made by the kidneys and drains via narrow tubes called ureters into your bladder where it is stored until you empty it by urinating through your urethra or “water pipe”. A stone may form in the kidneys causing problems like blockage and pain. In these cases doctors recommend that the stones must be removed.
What is a percutaneous nephrolithotomy (PCNL)?
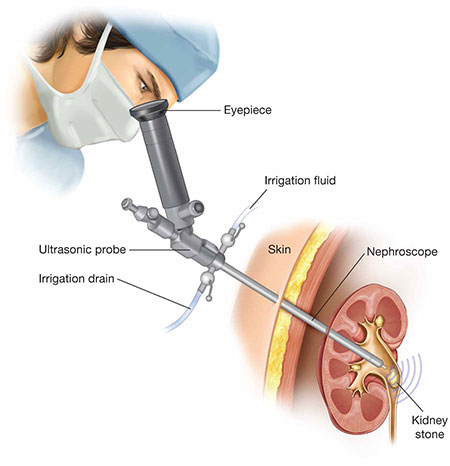
A percutaneous nephrolithotomy (PCNL) is a procedure to remove a kidney stone or stones. Percutaneous means ‘through the skin’ and nephrolithotomy means ‘taking stones out of the kidney’. The surgery is done telescopically.
This involves placing a kidney telescope called a nephroscope into the kidney via a small opening (incision) in the skin and using this instrument to remove the kidney stone(s). PCNL is a keyhole nephroscopic surgery.
How can a PCNL help me?
From the results of your tests, your doctor has confirmed that you have a stone or stones in your kidney. Not all kidney stones cause symptoms, but yours may have caused significant problems, such as pain, renal failure, or infection. If nothing is done to remove them, they will continue to grow and could damage your kidney.

What are the advantages of keyhole nephroscopic surgery?
- Less blood loss: in the keyhole operation, blood loss is typically much less than open surgery. Therefore, there is less risk of needing a blood transfusion with keyhole nephroscopic surgery.
- Less pain after the operation: as there is no large abdominal wound, patients need less strong painkillers following keyhole surgery and can return to normal activities and work sooner compared to open surgery.
- A shorter stay in hospital: most patients go home two to three nights after keyhole surgery, compared to an average of five to seven nights for open surgery.
- Smaller scars: the keyhole operation avoids the large scar from open surgery, although the smaller scar from where the telescope enters the skin will be visible.
- High success rate: ranging from 90-100%, depending on characteristics of stones.
What are the risks of having a PCNL?
Although this procedure has proven to be very safe, as in any surgical procedure there are risks and potential complications. Potential risks include:
- Bleeding in or around the kidney: some bleeding is normal; rarely, it may be significant enough to need a blood transfusion (in less than 5% of cases). If the bleeding does not stop it may be necessary to have a special interventional X-ray procedure called angiogram during which the interventional radiologist may obstruct the vessel that is bleeding in order to stop the haemorrhage. In the rare event that this does not stop the bleeding it can be necessary to remove the kidney (nephrectomy). This is extremely rare and happens in less than 1 in 1,000 cases;
- Infection: because some stones have bacteria trapped within them, we give you antibiotics routinely to prevent infection after the operation. A raised temperature is common (25%) after this procedure, but this is usually temporary. There is a 0.5% risk of sepsis (blood poisoning);
- Retained fragments: sometimes it is not possible to remove all of the stone during the operation, and in these cases usually it will be necessary to undertake further treatment. This may involve either Extra-corporeal Shock Wave Lithotripsy (ESWL) or surgical removal via the ureter (flexible ureteroscopy) or rarely repeating PCNL. Occasionally, to aid further treatments and ensure urine drains safely from the kidney to the bladder, a ureteric stent (a small hollow tube which goes down your ureter and into your bladder) is inserted at the end of PCNL;
- Fluid build-up: rarely fluid can leak from the kidney after surgery resulting in a collection of fluid inside your abdomen. If this becomes a large collection it may need draining. This is usually done in the X-ray department. In some cases a ureteric stent may also need to be inserted. Ureteric stents are left in temporarily until problems have been resolved and can then be removed usually within six weeks;
- Surrounding organs injuries.
Common risks (greater than 1 in 10):
- Temporary insertion of a urethral bladder catheter (tube draining urine from the bladder via your waterpipe) and ureteric stent/ kidney tube needing later removal;
- Temporary blood in the urine;
- Temporary raised temperature.
Occasional risks (between 1 in 10 and 1 in 50):
- Occasionally more than one puncture site is required;
- No guarantee of removal of all stones and need for further operations;
- Recurrence of new stones;
- Failure to successfully access the kidney resulting in the need for further surgery.
Rare risks (less than 1 in 50):
- Severe kidney bleeding requiring transfusion, embolisation or at last resort surgical removal of kidney
- Damage to lung, bowel, spleen, liver requiring surgical intervention
- Kidney damage or infection needing further treatment
- Over-absorption of irrigating fluids into blood system causing strain on heart function.
What will happen if I choose not to have PCNL?
If you decide not to have a PCNL, the doctor will talk to you about your options. Keep in mind that some alternatives may not give as good an outcome as PCNL or you may not be suitable to have the alternatives. Not having the treatment may result in long term damage to the kidney.
What alternatives are available?
The consultant caring for you has recommended that a PCNL is the most suitable option to remove your stone(s). However there are some alternatives. Possible alternatives include:
- Extracorporeal Shock Wave Lithotripsy (ESWL): this involves shattering your stones using shock waves. The stones break up into smaller fragments which you then pass out in your urine. This is usually done as an outpatient;
- Retrograde ureteroscopic laser lithotripsy: a telescope is put up your waterpipe, into your bladder and up the ureter into the kidney. The stone can then be grabbed with a special instrument, or shattered using laser and then the fragments removed;
- Open surgery: this involves the stones being removed via an opening in your side rather than using the telescope via the skin as in PCNL.
A PCNL generally removes more stone fragments than ESWL and has a shorter recovery time than open surgery. However, this will depend on your individual circumstances e.g. the size of the stone and where it is positioned in your kidney. Your consultant will discuss these alternatives with you in more detail if they are appropriate for you. Please ask questions if you are uncertain.
Asking for your consent
We want to involve you in all the decisions about your care and treatment. If you decide to go ahead with treatment, by law we must ask for your consent and will ask you to sign a consent form. This confirms that you agree to have the procedure and understand what it involves. Your doctor will explain all the risks, benefits and alternatives before asking you to sign a consent form. If you are unsure about any aspect of your proposed treatment, please don’t hesitate to ask more questions to your doctor.
How should I prepare for a PCNL?
You will have a consultation with an anaesthesiologist within a few days before your surgery. We will carry out a number of tests to make sure that your heart, lungs and kidneys are working properly. We will check that your urine is sterile: urinary infection, if any, must be treated prior to the surgery.
If you smoke, you may be asked to stop smoking, as this increases the risk of developing a chest infection or Deep Vein Thrombosis (DVT). Smoking can also delay wound healing because it reduces the amount of oxygen that reaches the tissues in your body.
Do not take aspirin or any drug containing aspirin for seven days prior to your surgery; avoid anti-inflammatory drugs like Advil or Ibuprofen for 24 hours prior to surgery. Stop any over the counter supplements, vitamin E and herbal medicines one to two weeks before surgery (current research indicates that vitamin E and some herbs inhibit clotting).
If you regularly take medications prescribed by your doctor (for example for diabetes, high blood pressure or other conditions), please inform the anaesthesiologist during the pre-surgery consultation. These medications are often to be taken as prescribed but, during the six hours prior to your procedure, only with a small sip of water.
You must not eat or chew gum or drink milk or fruit juice with pulp before six hours, and do not drink clear water, tea, coffee with or without sugar for two hours before your surgery. You must not smoke or drink alcohol for 24 hours prior to surgery.
What happens during a PCNL?
A telescope is placed through an incision which allows us to see pictures of the inside of your kidney on a High Definition (HD) monitor in the operating theatre.
This operation is carried out under general anaesthetic, which means you will be asleep throughout the procedure.
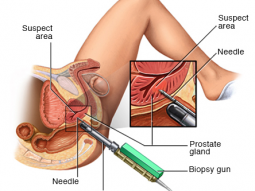
The operation begins by inserting a telescope-like instrument (known as a cystoscope) into the bladder. A tube is then passed up the ureter into the kidney. This tube allows the kidney to be filled with dye (contrast medium) to allow your surgeon to see the kidney on the X-rays.
You are moved into a prone position (lying face down). With the aid of X-ray or ultrasound, the kidney is punctured with a fine needle through your back. The needle position is confirmed by either outflow of urine or dye from the needle. Once the kidney has been entered, a 1cm incision is made in the back and the needle tract into the kidney is then stretched (dilated) to allow a telescope to be passed into the kidney. A scope and other stone fragmentation tools such as a laser or an ultrasonic probe will be inserted through this tract for stone fragmentation and removal. The whole procedure usually takes two to four hours.
After the operation, a tube may be left in the kidney and a catheter may be left in the urethra (the tube which carries urine from your bladder and out of your body) to ensure good urinary drainage. If present, these tubes are removed over the next few days depending on clinical progress and will be reviewed daily by the medical team.
What should I expect after a PCNL?
Once your procedure is over you will be taken to the recovery room and remain there until you come around from the anaesthetic. This may take an hour or two. You will then be taken to your ward. If you are in pain or feel nauseous (sick) while in the recovery room, please let the staff know, as they can give you medicine to help with this.

You will need to remain in bed at first. During this time, we will ask you to move your feet and ankles and wiggle your toes to help encourage circulation in your legs. This and deep breathing will also reduce the risk of blood clots in your legs. Deep breathing also helps to prevent lung problems after your surgery.
If you have a drainage tube from your kidney, it will be attached to a collection bag to drain your urine. The urine will be blood-stained. The nurses will regularly empty the bag and measure the volume of urine produced. How long you need this tube depends on the amount of left-over fragments, clots, and other debris. It is often removed the day after your surgery, but you may need X-rays to confirm when it is ready to be removed. You may also have a urethral catheter for about the first 24 hours after your surgery. This is a tube inserted into the bladder through your urethra (tube that carries urine from the bladder and out of the body). This may be uncomfortable; please tell us if it is so we can manage your discomfort.
The average stay in hospital for this surgery is two to three days after the operation.
What should I expect when I go home?
- You may experience some blood in your urine for up to two weeks. Make sure you drink plenty of fluids to help with this. Aim to drink two to three litres of water, squash or fruit juice each day. We recommend that you do not drink more than two cups of tea or coffee each day. We suggest that you avoid drinking alcohol while you are recovering.
- You may feel sore around the operated area for several weeks; we will prescribe you painkillers to help with this.
- Avoid becoming constipated by eating a healthy, balanced diet, as straining to open your bowels increases the risk of bleeding. Eat plenty of fruits and vegetables and other foods high in fibre, such as wholemeal bread, pasta and rice. If you need more advice about your diet, please speak to your doctor or nurse.
- Avoid lying down for long periods, as reduced movement increases the risk of developing pneumonia or blood clots in your legs.
- Avoid heavy lifting and straining for four weeks.
- The dressing over the wound site should be changed daily and the site inspected for healing. Never leave a wet dressing in place. Once the wound is dry and healed (usually within three–five days) the dressing can be removed.
- Give yourself two to four weeks before returning to work. If your work involves heavy lifting or exercise, please speak to your consultant.
- Only start driving again when you are able to perform an emergency stop without feeling hesitant.
- You may begin sexual activity again two weeks after your operation, as long as you feel comfortable.
How will I know the result?
- Your urologist probably will want to see you again after four to six weeks. At that visit, your doctor may use ultrasound or X-rays to check for any stones that may be left and to make sure that urine is draining normally from the kidney.
- Your urologist will also want to do some other tests to help determine what caused the kidney stones. You will also discuss ways to prevent getting more kidney stones in the future.
After the procedure when should I contact my doctor?
Please contact your doctor if you experience any of the following after you have left hospital:
- Persistent bleeding or leaking of urine from the operation site;
- Fresh blood in your urine;
- Excessive pain;
- A temperature over 38ºC;
- Difficulty passing urine;
- Any other problems that concern you.
Contact details
For further enquiries and appointment, please contact the Urology Department – FV Hospital at: (028) 54 11 33 33 – ext : 1032

 Vi
Vi