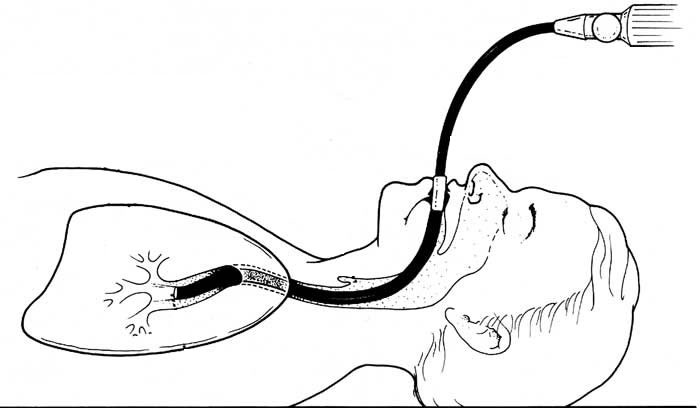
A flexible bronchoscopy (or fiberoptic bronchoscopy) is a procedure that allows the doctor to view the respiratory tract through a fiberoptic tube (bronchoscope), a thin tube-like instrument with a mini camera at its tip. This procedure enables the doctor to collect samples of mucus or lung tissues. It may also be used to remove an inhaled foreign body such as peanut.
WHY A BRONCHOSCOPY?
There are many reasons for having a bronchoscopy. Common ones include: coughing up blood, a persistent cough that has not responded to the usual medications, infection of the lungs, and abnormal chest X-ray findings.
Diseases of the lung can be analysed with bronchoscopy by sampling the lung tissue through the use of a bronchoscope. Samples are sent to a laboratory for analysis, from which your doctor can make a diagnosis.
Adults sometimes, and more often children, may inhale foreign bodies, such as peanuts, denture parts, pins, etc. into the lung. Sometimes a special grasping device can be inserted into the lung through the bronchoscope to remove the object.
HOW DO I PREPARE FOR A BRONCHOSCOPY?
Usually, the test is done as an outpatient procedure, and you will go home the same day. Some patients may need to stay overnight in the hospital.
- Your doctor will explain the procedure and get your written consent.
- Before the procedure, blood tests are sometimes required.
- Do not eat or drink anything for 6 hours before the procedure, however you can have sips of water up to 2 hours before the procedure.
- Do not smoke before the procedure because this can reduce how much oxygen your blood can carry.
- It is important to tell your doctor in advance if you take blood-thinning drugs such as aspirin, warfarin, clopidogrel (Plavix), or diabetes medications as we will need you to temporarily stop taking these before your procedure.
You may be sleepy after the test, so you should arrange for transportation to and from the hospital.
Many people want to rest the following day, so make arrangements for work, child care, or other obligations.
HOW IS BRONCHOSCOPY PERFORMED?
A bronchoscope is a flexible tube with a camera at the end. The tube is passed either through the mouth or the nose, into the respiratory tract, through your windpipe (trachea), and then into your lungs. Going through the nose is a good way to look at the upper airways. The mouth method allows the doctor to use a larger bronchoscope.
- Before the procedure begins, an intravenous catheter will be placed. You will receive medication that will help you relax and reduce coughing and throat irritation. Dentures and/or plates will be removed.
- Your blood pressure, oxygen level and heart rate will be monitored using a cuff on your arm and a sensor on your finger. Oxygen will be administered through a tube in your nose.
- Next you will be assisted into the proper position, usually sitting facing the doctor, or lying on a couch.
- The doctor will spray a numbing drug (anaesthetic) in your mouth, and throat to decrease discomfort and gagging that can occur when the scope is inserted. If the bronchoscopy is done through the nose, numbing jelly will be placed on one nostril. The anaesthetic has an unpleasant taste and you will begin to feel your throat get numb, making you feel as if you can’t swallow, but you will still be able to.
- The bronchoscope will go down the back of your throat and into your breathing passages, and further local anaesthetic will be used to numb your voice box and your trachea.
- The doctor will examine your respiratory tract and collect samples using various methods:
- Saline (salty water) being flushed through the bronchoscope and sucked out again, to collect cells for analysis;
- Brush passed down the bronchoscope to brush cells for the lining of your air tubes;
- Special forceps on the end of a wire used to take small biopsies (no bigger than 2-3 mm).
WHAT HAPPENS AFTER BRONCHOSCOPY?
When the procedure is finished, you will be observed by a nurse in a recovery area until the sedative has worn off and you are awake enough to leave. Tell the nurse if you have any chest pain, difficulty breathing, or notice a large amount of blood (more than one tablespoon) in your sputum. It is normal to cough after a bronchoscopy and there may be a small amount of blood in your sputum for few days. A sore throat, sore nose, mild headache, fatigue and a delayed fever (several hours) can also develop after the procedure.
The nurse will recheck your blood pressure, pulse, and respiratory rate prior to your discharge. The IV needle will be removed.

You will also need to wait until the numbing medicine wears off before drinking any liquids. This could take 1 to 2 hours.
Smoking after having a bronchoscopy is discouraged, as it will increase irritation in respiratory tract.
WHAT ARE THE RISKS?
Bronchoscopy is a safe diagnostic procedure and carries little risk. Complications are infrequent, but if they occur, they may include:
- Discomfort and coughing: While the bronchoscope is passed through the nose, throat and breathing tubes, it may cause some discomfort. It may also tickle the airways leading to cough. Doctors try to reduce this discomfort and coughing with local anaesthetics. To decrease these discomforts, medications are sometimes given to relax patients or make them sleepy.
- Lung leak: rarely, an airway may be injured by the bronchoscope, particularly if the lung is already very inflamed or diseased. If the lung is punctured, it may cause an air leak (called a pneumothorax). The air leaks around the lungs and can cause the lung to collapse. This complication is not common, and is more likely if a biopsy is taken during bronchoscopy. If there is a large or ongoing air leak, it may need to be drained with a chest tube.
- Reduced oxygen: the level of oxygen in the blood may fall during the procedure for several reasons. The bronchoscope may block the flow of air into the airway, or small amounts of liquid used during the test may be left behind, causing the oxygen level to drop. This drop is usually mild, and the level usually returns to normal without treatment. If the oxygen level remains low, the doctor will give extra oxygen or stop the test to allow for recovery.
- Bleeding can occur after a biopsy is obtained or if the bronchoscope injures a tumour in the airways. Bleeding is more likely if the airway is already inflamed or damaged by disease. Usually bleeding is minor and stops on its own. Sometimes a medication can be given through the bronchoscope to stop bleeding. Rarely, bleeding can lead to severe breathing problem.
WHEN TO EXPECT THE RESULTS?
After the procedure your doctor will discuss some of the initial results with you. The specimens are sent to the lab for testing. It can take approximately 7 to 10 days for the final results on your tissue investigations; some results may be available sooner.
You usually will need to come back to see your doctor to discuss the results a few days after the procedure.

 Vi
Vi