CONGRATULATIONS ON YOUR PREGNANCY
A pregnancy is both a happy and challenging journey in the life of any women. To experience a healthy and safe pregnancy, as well as to give your baby the best beginning in life, mothers-to-be must undergo regular follow-ups during their pregnancy to prevent and deal with potential complications in a timely manner. With this in mind, FV Hospital has devised a comprehensive package that cares for your health and that of your baby at every stage of your pregnancy.
The department of Obstetrics & Gynaecology of FVH is fully equipped with advanced, cutting-edge equipment to ensure mothers-to-be benefit from world-class care within a comfortable, welcoming environment. Our dedicated team of healthcare professionals, which includes obstetricians, midwives and anaesthesiologists, will help you to remain in good health and ensure any problems you or your baby may experience are discovered and addressed at the earliest opportunity.
Although every mother-to-be should see their doctor from the start of their pregnancy, it is never too late to start a pregnancy follow-up package. Even if your pregnancy is well advanced and you have not yet seen a medical practitioner or if you commenced your pregnancy care at another hospital and would like to continue the programme at FVH, we will ensure that you will receive the best care possible and that all necessary tests are conducted.
- Consultations with obstetrician, midwife and anaesthesiologist
- Antenatal screening
- 3D/4D ultrasound scanning
- Screening for various infectious diseases and routine blood and urine testing
- Foeto-maternal monitoring
YOUR FIRST CONSULTATION
As soon as you suspect that you are pregnant, you should make an appointment with an obstetrician. Even if you are not a first time mother, prenatal visits are still very important as every pregnancy is different.
FV Hospital’s pregnancy follow-up consultations are scheduled at key stages of your pregnancy, and the first consultation included in the follow-up package takes place between week 11 to week 13 and 6 days, counted from the first day of your last period.
Your initial visit will probably be one of the longest and it would be helpful to bring any information you have about your medical history, general health and previous pregnancies. Please do not omit to tell your doctor about any current or past health problems you have experienced, such as hypertension or diabetes, and let your doctor know if you have breast implants.
Your doctor will ask you questions about your medical history, including details of the following:
- Medical and/or psychosocial problems
- Blood pressure, height, and weight
- Recent breast and cervical examinations
- Date of your last menstrual period (an accurate date is helpful in order to determine gestational age and your due date)
- Birth control methods
- History of abortions and/or miscarriages
- History of hospitalisations and surgeries
- Medications you are taking
- Medication allergies
- Your parents’ and grandparents’ medical history (understanding your family medical history is important as some conditions are hereditary)

There are many things in our day-to-day lives that we don’t give much thought but which may have an impact on a pregnancy and an unborn foetus. Mothers-to-be should be aware of these new considerations, so during your first consultation your doctor will also want to discuss the following:
- Recommendations concerning dental care, cats, raw meat, fish, and gardening
- Fevers and medications
- Environmental hazards
- Travel limitations
- Miscarriage precautions
- Diet, exercise, nutrition, weight gain
Your first consultation is also a good opportunity to bring a list of questions that you and your partner may have about your pregnancy, prenatal care and birth options. Possible questions to ask your doctor include:
- Can I call to speak to a midwife if I have any questions or problems?
- If I experience bleeding or cramps, should I call you or a midwife?
- What do you consider an emergency?
- Will I need to change my habits regarding sex, exercise and nutrition?
- When will my next prenatal visit be scheduled?
During this first consultation your doctor will give you your personalised Pregnancy Due Date Calculator and Schedule of Consultations.

Your doctor will give you the dedicated FVH phone number for pregnant women (Obstetrics Hotline 24h/24h (028) 54 11 34 50) and will explain to you why we created this service.
During this first consultation or later in your pregnancy you will have the opportunity to discuss labour and delivery issues with your doctor, and also with the midwife during the consultation with her (between the 21st and the 23rd weeks). Some questions to ask regarding labour and delivery include:
- Can you explain things I need to be aware of when considering a natural birth?
- What situations would warrant a caesarean section (c-section)?
- What situations would warrant an episiotomy (surgical incision to the perineum)?
- How long past my expected due date will I be allowed to go before an intervention is necessary?
- What is your policy on labour induction?
FVH PREGNANCY FOLLOW-UP PACKAGE
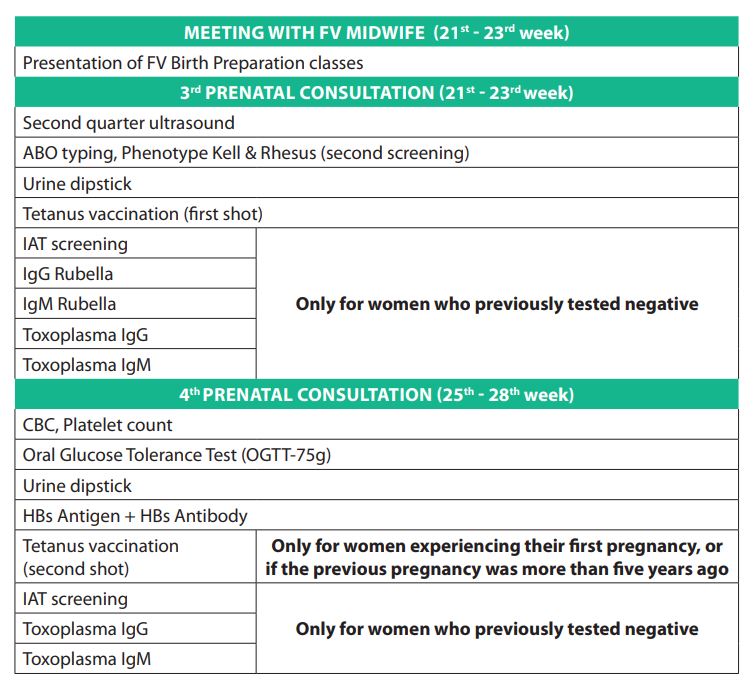
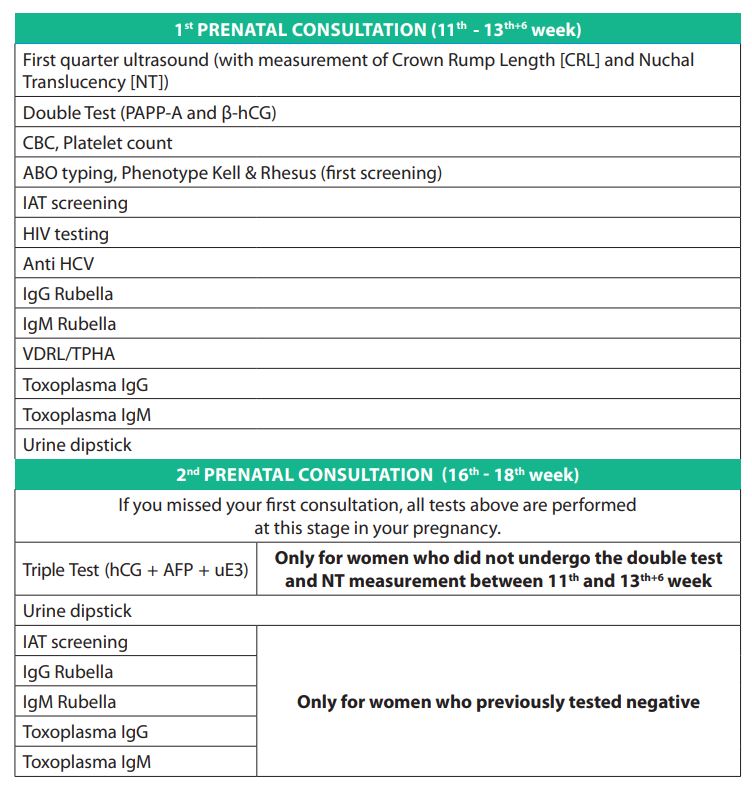
PRENATAL TESTS
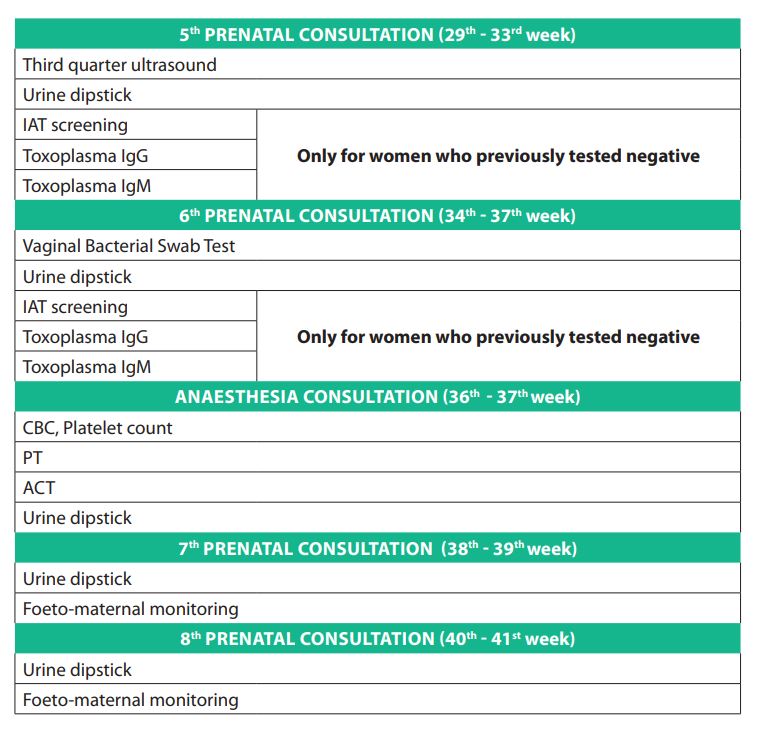
Prenatal tests are medical tests performed during pregnancy. They enable your obstetrician to ascertain how you and your baby are doing. Some of these tests, such as blood pressure checks and urine tests, are routine. you will undergo these tests at almost every check-up. other tests are performed at specific times during your pregnancy to check that your baby is developing normally, or when prescribed by your doctor to address a specific issue.
1) ULTRASOUND SCANNING
Ultrasound scanning is performed by a team of dedicated ultrasonographers, each with more than 10 years of experience in prenatal ultrasonography, certified by the Fetal medicine Foundation in London.
The first ultrasound study takes places between the 11th and 13th weeks + 6days to measure your baby’s Crown rump Length (CrL) in order to identify gestational age and the nuchal translucency (NT). NT measurement is combined with specific blood tests for the screening of Down syndrome (see below).
The second study is done between the 21st and the 23rd weeks, using 3D reconstructions and real-time 4D imaging. This ultrasound study gives parents a unique opportunity to see their baby’s image before birth, helping them to bond and establish an early relationship.
During the third trimester ultrasound (29th to 33rd weeks) the ultrasonographer checks the development of the foetal organs, the location of placenta and assess foetal growth speed.
in addition your obstetrician can perform an ultrasound at any stage of your pregnancy straight in the consultation room.

2) ANTENATAL SCREENING FOR DOWN SYNDROME
Screening for Down syndrome is offered as a routine part of prenatal care to all pregnant women, regardless of age.
First Trimester Combined Screening Test
The Combined Test must be performed between week 11 to week 13 and 6 days, counted from the first day of your last period. The Combined Test gives detection rates for Down syndrome of 85-90% and false positive rates of 5%. it includes:
- Ultrasound scanning to measure a specific region on the back of a baby’s neck. This is known as a nuchal translucency (NT) screening test. When abnormalities are present, more fluid than usual tends to collect in this tissue.
- The double Test which measure levels of pregnancy-associated plasma protein-a (PaPP-a) and a hormone known as human chorionic gonadotropin (HCg) in the maternal blood.
Triple Test
if the Double Test has not been performed or not in time, the Triple Test must be done between week 16 to week 18. This test measures the level of human chorionic gonadotropin (βhCg), alpha-fetoprotein (aFP) and unconjugated estriol (uE3) in the maternal serum. Like the Double Test it must be combined with the ultrasound nuchal translucency (NT) screening test.
Diagnostic tests
If your screening test results are positive or worrisome or you are at high risk of having a baby with Down syndrome, you might consider further testing to confirm the diagnosis. These diagnostic tests are not included in the FVH Pregnancy Follow-up package. There are three types of diagnostic tests that can identify Down syndrome:
- Amniocentesis. a sample of the amniotic fluid surrounding the fetus is withdrawn through a needle inserted into the mother’s uterus. This sample is then used to analyze the chromosomes of the fetus. Doctors usually perform this test after 15 weeks of gestation. The test carries a 1 in 200 risk of miscarriage.
- Chorionic villus sampling (CVS). Cells taken from the mother’s placenta can be used to analyze the fetal chromosomes. Typically performed between the ninth and 14th week of pregnancy, this test carries a 1 in 100 risk of miscarriage.
- Cordocentesis also called percutaneous umbilical blood sampling (PUBS). Blood is taken from a vein in the umbilical cord and examined for chromosomal defects. Doctors generally perform this test after 18 weeks of gestation. This test carries a greater risk of miscarriage than does amniocentesis or chorionic villus sampling. generally, this test is only done when results of other tests are unclear.
3) BLOOD TESTING
a) Complete blood cell count
This blood test can tell if your haemoglobin levels are low, which is a sign of anaemia. if you are anaemic, your obstetrician will talk to you about the best foods to eat. you might also be prescribed iron tablets.
b) ABO typing, Rhesus factor (Rh) and kell phenotype
Every human being is one of four blood types, a, B, aB or o, and is either rh negative or rh positive. aBo and rhesus typing are carried out twice so that if you haemorrhage during delivery, we have a double determination of your aBo and rh type for blood transfusion purposes.
if you do not have the rh antigen in your blood, you are rh negative; if you do have it, you are rh positive. This test is important because problems may arise if the mother’s blood does not have the rh factor and the baby’s blood does. if you have rh negative blood type, your doctor will screen for irregular antibodies every month. an injection of anti-D gamma-globulines may be proposed at 28 week to prevent any rhesus antibodies forming. if your baby at birth is rhesus positive and you are rhesus negative your doctor will prescribe you one injection of anti-D during the first 24 hours after birth to prevent any risk of immunization in a subsequent pregnancy .
one Kell antigen, K (KEL1), has the potential to cause problems for the foetus and newborn and we routinely test for it.
c) Sexually Transmitted diseases
Your blood will be tested to determine whether you have syphilis, hepatitis C , hepatitis B, or HIV.
- The VDrL/TPHa test for syphilis is performed early during your pregnancy. if the result is positive, your doctors will prescribe a course of antibiotics.
- HIV Testing must also be carried out with your consent early in the pregnancy. if the test is positive, your pregnancy will be followed up and treated by specialists to prevent mother-to-child transmission.
- If you are positive for anti HCV (Hepatitis C), you will be seen by a hepatologist (liver specialist) who will decide whether you need a specific treatment for hepatitis C.
- Tests for HBs antigen and HBs antibody are performed from week 26 to 28 of the pregnancy. if your ag Hbs result is positive, you will be seen by a hepatologist who will decide whether you need a specific treatment for hepatitis B. FVH provides vaccination against hepatitis B for all newborns during the first 24 hours of life. For newborns whose mother is ag HBS positive, this vaccination will be carried out in the Delivery Suite and gamma globulines will be given to your baby.

d) Rubella
Most pregnant women are immune to rubella (have antibodies for rubella in their blood) because they have either been vaccinated against it or they have had the disease as a child. if you do not have rubella antibodies this test will be performed monthly from your first consultation to week 20 of your pregnancy.
If you are not immune you’ll be advised to avoid anyone who has or might have the infection. if a woman becomes infected by the rubella virus within the first 20 weeks of pregnancy, the risks of congenital rubella Syndrome, with congenital anomalies especially congenital heart defects, are extremely high and there is no effective treatment. in such a case termination of the pregnancy will unfortunately be advised by the obstetrician.
After 20 weeks, the foetal organs have fully developed so even if you are infected with rubella virus at this stage, there is no longer any risk of congenital rubella Syndrome.
e) Toxoplasmosis
You blood will be tested for toxoplasmosis (Toxoplasma antibodies), an infection caused by the parasite Toxoplasma gondii. While toxoplasmosis is harmless to you, it may cross the placenta and cause increased risk of miscarriage or birth defects.
If you have no toxoplasmosis antibodies, your doctor will explain hygiene rules that you should follow to prevent the risk of parasite infection. if test results suggest that you got toxoplasmosis while pregnant, your practitioner may begin treating you with an antibiotic that may lower your risk of transmitting the infection to your baby. and since not all maternal infections are transmitted to the baby, you may have an amniocentesis to determine whether your baby also has the infection.
f) Glucose Tolerance Test
The glucose tolerance test, conducted in the 25 to 28 weeks of pregnancy, measures levels of sugar (glucose) in the mother’s blood. abnormal glucose levels may indicate gestational diabetes. if you have gestational diabetes, your obstetrician will make you an appointment with one of FVH’s nutritional specialists and an endocrinologist.
4) URINE TEST DIPSTICK
your obstetrician will ask you for a urine sample at each of your prenatal visits. a quick dipstick test will be done on your urine sample to check for the following things:
Sugar
It is normal to occasionally have a small amount of sugar in your urine during pregnancy, but if you have elevated levels at a couple of prenatal visits in a row or a very high level at one visit, it could mean you have gestational diabetes. your practitioner may have you take a glucose tolerance test to find out whether that is the case. (Even if your urine test results are normal, you’ll have a glucose challenge test between 25 and 28 weeks to check for this relatively common condition.)
Protein
Excess protein in your urine can be a sign of a urinary tract infection, kidney damage, or certain other disorders. Later in your pregnancy, it can also be a sign of preeclampsia if it is accompanied by high blood pressure. if you have protein in your urine but your blood pressure is normal, your sample will be sent to the lab for a culture to see whether you have an infection.
Ketones
Ketones are produced when the body starts breaking down stored or ingested fat for energy. This can happen when you are not getting enough carbohydrates (your body’s usual source of energy). if you’re suffering from severe nausea and vomiting or you’ve lost weight, your practitioner may check your urine for ketones. if your ketone reading is high and you can’t keep any food or liquid down, you may need intravenous fluids and medication. if ketones are found in combination with sugar, it could be a sign of diabetes.

5) GROUP B STREPTOCOCCUS COLONISATION TEST
GBS infection usually causes no problems in women before pregnancy, but can cause illness in the mother during pregnancy such as chorioamnionitis (an infection of the placental tissues) and urinary tract infections that can lead to pre-term labour and birth. gBS is the most common cause of life-threatening infections in newborns, including pneumonia and meningitis. Newborn babies can contract the infection during pregnancy or from the mother’s genital tract during labor and delivery.
FVH recommends screening of all pregnant women for vaginal gBS colonization between 34 to 37 weeks’ gestation. in case of colonization you will be given, during labour, an antibiotic treatment to reduce the risk of transmission of gBS to the baby. Babies whose mothers receive antibiotic treatment for a positive gBS test are 20 times less likely to develop the disease than those without treatment. in case of suspicion of gBS infection of the newborn a 2-day antibiotic treatment will be administered, if the infection is confirmed the treatment will last 7 days.
6) TETANUS VACCINATION
in line with the Ministry of Health regulations, all pregnant women must receive a tetanus vaccination between weeks 21 and 23 of their pregnancy. a “booster” injection, between weeks 25 and 28, is required only for women having a first pregnancy or if the previous pregnancy was more than 5 years ago.
TWO IMPORTANT PERSONS TO SEE

1) YOUR MIDWIFE
This 45-minutes meeting gives you the opportunity to discuss your pregnancy, labour, delivery, newborn care and postpartum recovery. The father is encouraged to attend this meeting.
Your midwife will also explain to you the FVH childbirth classes organised with FVH’s midwives and paediatric nurses, nutrition specialists, physiotherapists, psychologists and anaesthesiologists. These classes have been devised to further explain to mothers-to-be and their partner key aspects of the pregnancy and practice delivery techniques for a small fee. Please call (028) 54 11 33 40 or ask your doctor during any pregnancy consultation for more information.
2) THE ANAESTHESIOLOGIST
You will see a FVH anaesthesiologist once you reach week 36 of your pregnancy (around one month before you are due to deliver). During this consultation, the anaesthesiologist will explain obstetric pain control techniques and indicate some tests (at the minimum complete blood cell and platelet count, coagulation tests, urine dipstick). Pre-anaesthesia tests must be conducted less than one month prior to delivery.
FOETO-MATERNAL MONITORING

During late pregnancy and during labor, your obstetrician will ask the midwife to perform foeto-maternal monitoring. This monitoring is done by placing external sensors on the mother’s abdomen, secured with elastic straps. one sensor is using doppler ultrasound to monitor foetal heart rate, the other one is used to record uterine contractions. The average foetal heart rate is between 110 and 160 beats per minute. The foetal heart rate may change as the fetus responds to conditions in the uterus. an abnormal foetal heart rate or pattern may mean that the fetus is not getting enough oxygen or there are other problems. During labour an abnormal pattern also may mean that an emergency or cesarean delivery is needed.
PREGNANT WOMEN WHO WERE NOT FOLLOWED AT FV HOSPITAL

If you have undergone your pregnancy follow-up at another healthcare facility but wish to deliver your baby at FV Hospital, please bring with you all your laboratory and ultrasound test results (blood type, CBC, irregular antibodies screening, rubella igg/igM, Toxoplasmosis igg/igM, HBs antigen and HBs antibody, anti HCV, HiV testing, triple test, urinary tests, etc.).
Additional tests and treatments may have to be performed if the obstetrician and the anaesthesiologist deem them necessary for your safety and that of your baby.
Thank you for choosing FV Hospital as your healthcare provider and your dedicated partner for this exciting journey into motherhood. We are proud to offer you the best care possible to ensure you and your baby remain in the best of health.
For more information on FV’s Pregnancy Follow-up Package or to register for a Childbirth Preparation Class, please call: (028) 54 11 35 35 you may also refer to FVH’s antenatal brochure, available at FVH’s Obstetrics & Gynaecology Department.

 Vi
Vi