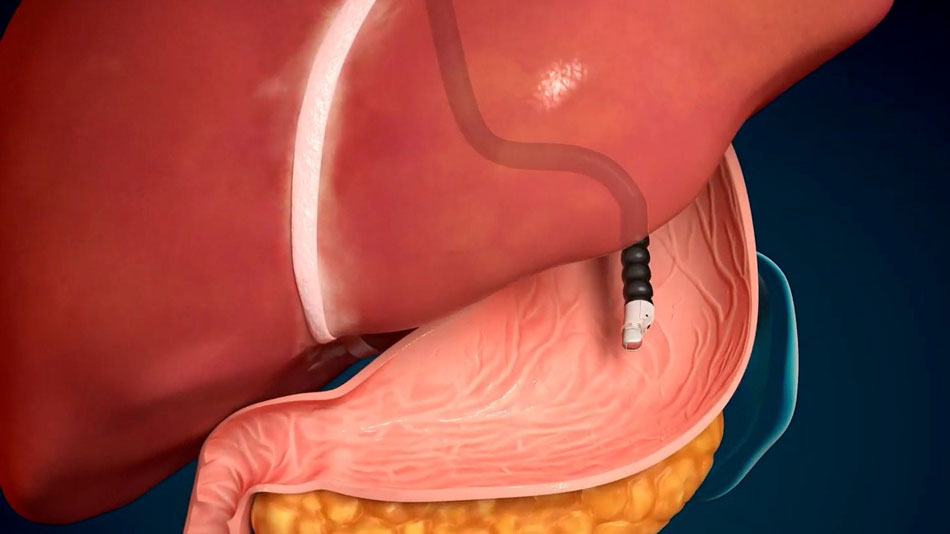
Combining the capabilities of ultrasound and endoscopy, endoscopic ultrasound (EUS) allows physicians to “see through” each layer of the gastrointestinal tract, providing accurate diagnosis of digestive disorders and enabling interventions such as sampling for pathological analysis and stent placement.
Colonic polyps—a common gastrointestinal disorder
After being diagnosed with a submucosal tumour and colorectal cancer at another hospital, Mr Nguyen Van N. (68 years old) visited FV Hospital for treatment. His CT scan results raised suspicion of a submucosal tumour in the rectal region, suspected transverse colon mass, multiple liver nodules, and multiple bilateral renal nodules, with mild prostatic hyperplasia (a pre-cancerous sign). Notably, the CT scan results did not indicate whether the submucosal tumour was malignant or benign.
Endoscopic ultrasound (EUS) can help detect submucosal tumours in the rectal region.
Bui Nhuan Quy, MD, MSc., Specialist Level II, Head of the Gastroenterology and Hepatology Department, FV Hospital, explains that submucosal tumours in the gastrointestinal tract originate from the muscle layer, submucosal layer, or muscularis propria. Most submucosal tumours are asymptomatic and are incidentally detected during endoscopy. Submucosal tumours account for about three per cent of patients presenting with gastrointestinal symptoms. To determine the appropriate treatment approach, Dr Quy emphasises the importance of distinguishing between benign and malignant (cancerous) submucosal tumours. However, due to their location within the intestinal wall beneath the mucosal layer, accurately diagnosing the nature of submucosal tumours through endoscopy or CT scan can be challenging.
In the past, patients may have undergone exploratory surgery to determine the nature of the tumour, which could be costly, inconvenient, and pose risks to their health.
FV Hospital’s doctors recommend patients undergo investigation using endoscopic ultrasound (EUS) to determine the nature of submucosal tumours and guide appropriate treatment without the need for exploratory surgery. Dr Bui Nhuan Quy, says that EUS plays a crucial role in allowing doctors to decide which is the best treatment approach and directly impacts the final outcome in such cases.
Dr Quy states that the ability of EUS to “see through” each layer of the gastrointestinal wall has made it a primary resource for providing additional data to evaluate the submucosal layer in this area. “EUS is the best tool for identifying the characteristics of submucosal tumours in the digestive tract, with a sensitivity of up to 92 per cent,” he adds.
Endoscopic Ultrasound (EUS) helps detect terminal gastrointestinal cancers.
Since 1980, Endoscopic Ultrasound (EUS) has been used worldwide, combining the features of endoscopy and ultrasound to provide a superior imaging method. This diagnostic technique utilises a flexible endoscope with an attached ultrasound probe at its tip, allowing the probe to be brought closer to the internal organs within the patient’s abdominal cavity.

Dr Bui Nhuan Quy explains the EUS technique to a patient.
EUS provides high-resolution, accurate imaging that can be combined with Doppler ultrasound to assess blood vessels and perform diagnostic procedures. With the support of EUS, doctors can also perform vascular interventions, fine-needle aspiration, and core biopsies for histological diagnosis. This technique is highly useful in detecting early-stage gastrointestinal cancers.
In Vietnam, this technique has been implemented in major public hospitals. FV is one of the few private hospitals to have pioneered the use of EUS. As a result, patients no longer need to undergo exploratory surgery and can instead undergo fine-needle aspiration (FNA) procedures to obtain tissue samples for pathological examination directly during the endoscopic ultrasound. This not only enables accurate diagnosis of the nature of gastrointestinal submucosal tumours but also minimises potential risks.
EUS has the potential for expanded applications in interventions and disease treatment.
In addition to accurately diagnosing the nature of submucosal lesions in the gastrointestinal tract, EUS is also a supplementary method to CT or MRI in diagnosing and staging pancreatic cancer. Current studies show that this technique has a sensitivity of 90 to 95 per cent in detecting malignant pancreatic tumours measuring 2-3 centimetres, which is significantly superior to other imaging modalities. EUS has also demonstrated excellent efficacy in diagnosing other conditions, such as chronic pancreatitis, pancreatic cysts, biliary stones, jaundice, gallbladder inflammation, and other gastrointestinal disorders.

Dr Bui Nhuan Quy says that EUS can be used for the treatment of many diseases.
Compared to other imaging diagnostic methods, EUS has a significant advantage in therapeutic interventions for diseases. A notable example is the intervention of local complications in acute pancreatitis such as acute fluid collection, pseudocysts, acute necrotic collections, and walled-off necrosis.
Previously, these cases would require surgical placement of drainage tubes to remove fluid through the skin. This method often comes with high costs, prolonged hospitalisation, a higher risk of secondary infections, and discomfort for the patient due to the external drainage tube which must be frequent replaced. With the assistance of EUS, the procedure of placing a transgastric or transcolonic drainage tube for pancreatic fluid has become widely performed in recent years with equivalent success and lower costs compared to percutaneous drainage surgery.
“EUS is feasible in over 90 per cent of patients, ensuring minimal invasiveness and a shorter hospital stay,” emphasises Dr Quy.
However, EUS is still an invasive intervention and comes with potential risks, such as sedation-related complications, perforation of the gastrointestinal tract, infection, pancreatitis, and bleeding. Therefore, this technique should be performed in healthcare facilities equipped with advanced and modern equipment, and by highly skilled physicians to minimise the occurrence of complications.
At FV Hospital, EUS is routinely performed by experienced physicians in the field of endoscopy and gastroenterology, led by Dr Bui Nhuan Quy, a specialist with many years of experience. With state-of-the-art equipment and standardized treatment protocols, the Gastroenterology and Hepatology Department at FV Hospital offer most complex EUS techniques, including diagnosing lesions and determining the stage of malignant diseases, performing fine-needle aspiration and biopsy for pathological examination, placing pancreatic cyst drainage into the stomach, placing transgastric transmural drainage, and placing biliary stents, among others.
To make an appointment and receive treatment for gastrointestinal disorders at FV Hospital, please contact: (028) 54 11 33 33.

 Vi
Vi