A Turkish woman experienced severe postpartum haemorrhage as a result of placenta accreta, requiring a life-saving hysterectomy. However, the patient and her husband firmly refused the surgery.
Caught between the need to save the patient’s life and respect her rights, how did FV doctors uphold medical ethics in this critical situation?
Vo Trieu Dat, MD, MSc, Head of the Obstetrics & Gynaecology Department, explained that this was a rare case in which a patient facing life-threatening haemorrhage refused a hysterectomy – the standard, life-saving treatment for such a condition. While respecting the patient’s rights, the medical team spent many hours explaining and persuading her to consent to the necessary treatment.

Persistently persuading the patient to secure necessary treatment.
Ms J.S., a 40-year-old mother, with a history of three previous deliveries, including a set of twins and multiple caesarean sections, visited FV Hospital at 33 weeks pregnant with her fourth child. Dr Vo Trieu Dat noted that all of her prior medical records from abroad had been lost.
On January 3, 2025, Ms J.S. was admitted at 3:30 PM and delivered a healthy baby boy weighing 3.4 kg just 30 minutes later. However, soon after delivery, she experienced significant vaginal bleeding. Despite an initial attempt to control the bleeding with a balloon tamponade procedure, the bleeding persisted, signalling postpartum haemorrhage. In response, the medical team decided to transfer the patient to the operating room to control the bleeding, with the possibility of performing a hysterectomy if necessary.
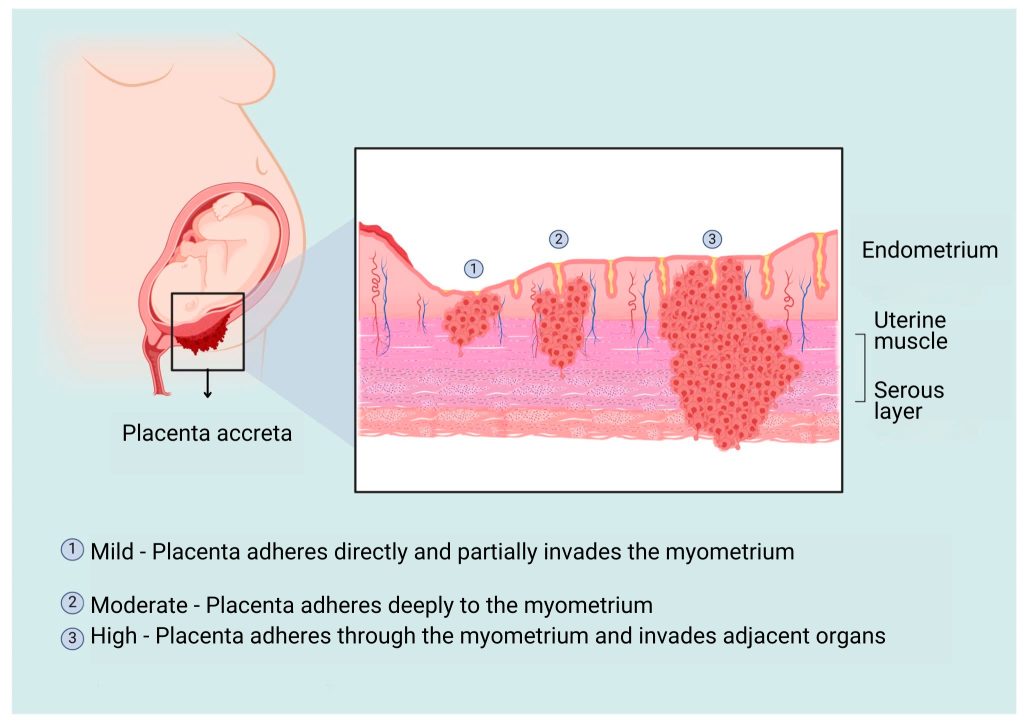
“Postpartum haemorrhage is a dangerous obstetric complication that can occur even in patients without risk factors. In Ms J.S.’s case, the haemorrhage was caused by placenta accreta near the old surgical scar. This is an extremely critical situation, and if not addressed promptly, the patient could lose a life-threatening amount of blood,” explained Dr Vo Trieu Dat.
However, the patient and her husband strongly opposed surgery, opting instead to remain in the delivery room under close observation. Despite their refusal, the entire surgical team, including anaesthesiologists and obstetricians, remained on standby, ready to perform the procedure at any moment.
“From 7:30 PM until 1:00 AM the following day, it was a tense mental battle between the medical team and the couple,” recalled Dr Dat. “We were deeply concerned for the patient’s life and tried our best to persuade them to accept treatment. Despite understanding the severity of the situation, they calmly insisted on continuing blood transfusions and monitoring.”
Dr Dat described the intense emotional strain as the patient began showing clear signs of haemorrhagic shock, including falling blood pressure and a rapid pulse. At times, she drifted into a semi-conscious state due to severe blood loss, but when alert, she remained resolute in refusing surgery. Her husband unwaveringly respected her decision. The medical team grappled with feelings of helplessness and frustration, torn between their duty to save her life and her right to decide her own treatment.
A temporary solution was attempted an embolization procedure to control the bleeding—but within 30 minutes, the haemorrhage resumed. The patient’s blood pressure dropped further, and she entered a critical state of shock.
When Life Takes Priority
Dr Dat observed the patient’s condition deteriorating rapidly. Despite their commitment to respecting the patient’s decision, immediate intervention was crucial to save the mother’s life. “We had no choice but to take the patient to the operating room immediately. At that moment, the priority had to be the patient’s survival, even though she had refused treatment,” Dr Dat recounted.
Mrs J.S. was urgently taken to the operating room, where Dr Dat once again consulted with her husband, explaining that a hysterectomy was the only option to stop the bleeding and save her life. Realizing the severity and urgency of the situation, her husband finally consented to the surgery.
The operation began at 1 AM, with Dr Dat performing a partial hysterectomy to successfully control the bleeding. The patient had lost a total of 2.5 litres of blood but, fortunately, responded well to the treatment and recovered quickly.
Dr Dat shared that, despite his extensive experience managing postpartum haemorrhage, this was the first time he encountered such a dramatic situation. “Thankfully, we were able to convince the family in the end,” he said.
Three days after being discharged, Mrs J.S. and her husband expressed their gratitude to FV’s medical team. They acknowledged the seriousness of the situation and recognised that the doctors had done everything in their power to save her life.
At FV, doctors approach every situation with professionalism, dedication, and responsibility, always respecting patients’ rights. However, when patients’ rights are weighed against their lives, saving lives always takes precedence. According to Dr Dat, this is the essence of medical ethics.


 Vi
Vi 












