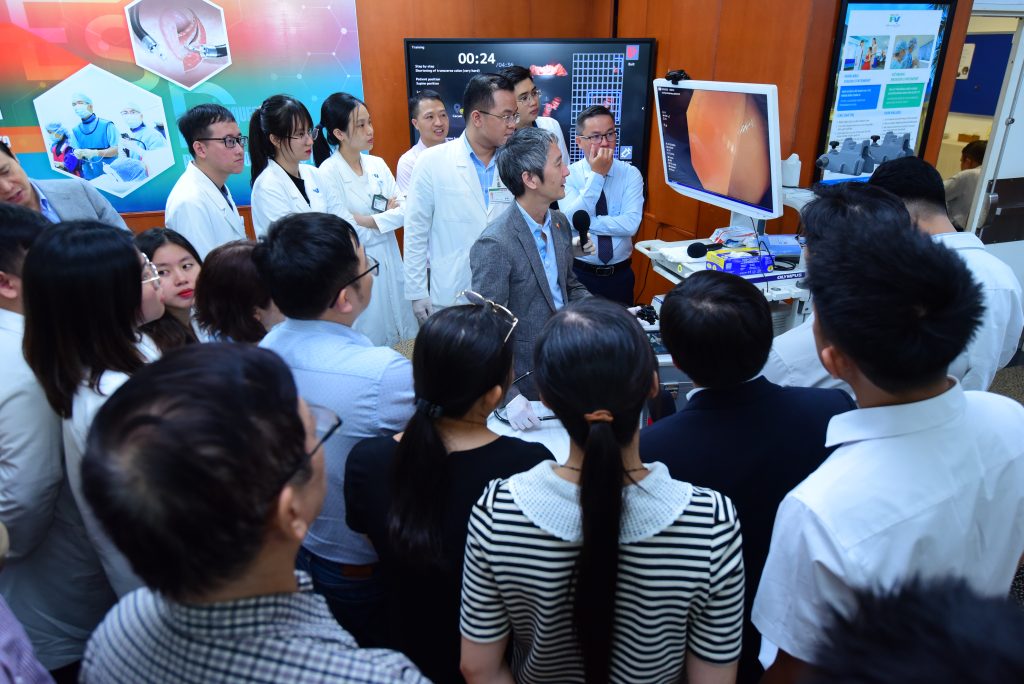
On 12 June 2025, FV Hospital hosted an advanced workshop titled “Enhancing Endoscopic Submucosal Dissection (ESD) Techniques,” led by Prof Tomohiko Richard Ohya, MD, PhD a renowned interventional endoscopy expert from Japan. The workshop also featured senior gastroenterologists from FV’s Gastroenterology & Hepatology Department and welcomed more than 50 participants, including doctors, nurses, and technicians. The programme delivered the latest advancements in ESD techniques, and provided hands-on practice using the MIKOTO model and pig stomach specimens, helping participants bridge the gap between theory and clinical application.

The programme opened with a speech by Vu Truong Son, MD, MSc – Medical Director of FV Hospital, who reaffirmed FV’s commitment to continuous medical education, particularly in specialised fields such as interventional gastrointestinal endoscopy. He highlighted that this workshop offered a valuable opportunity for participating doctors to gain hands-on experience with advanced ESD training models, moving closer to the standards of early-stage gastrointestinal cancer treatment commonly practiced in Japan.
The first presentation was delivered by Dr Ngo Van Huy, Deputy Head of the Gastroenterology & Hepatology Department at FV, who provided an overview of the ESD programme and its training objectives. He explained that ESD is a minimally invasive technique developed in Japan in the late 1990s, designed to precisely remove large polyps or early-stage cancerous lesions in the gastrointestinal tract without the need for open surgery.

With the ability to completely remove lesions confined to the mucosal layer while preserving the integrity of the gastrointestinal tract, ESD helps patients avoid major surgery, reduce pain and complications, shortens hospital stays, and supports faster recovery. It is considered an optimal treatment for improving quality of life, especially in the management of early-stage oesophageal, gastric, and colorectal cancers. Dr Huy noted that ESD has been performed at FV Hospital for over five years, and that mastering this advanced technique requires significant training and practice.
A key highlight of the workshop was the series of in-depth clinical presentations delivered by Prof Ohya, an interventional endoscopy expert from Japan. In his first session, Prof Ohya focused on the use of Narrow Band Imaging (NBI) technology in detecting early-stage cancers of the oesophagus, stomach, and colon – a major challenge in diagnostic endoscopy. He shared practical tips for recognising abnormalities based on microstructural features, including surface and vascular patterns.

In the advanced section on ESD session, Prof Ohya provided a detailed walkthrough of the procedural steps, including lesion marking, initial incision, submucosal dissection, and complete removal of the lesion. He also shared strategies for performing ESD tailored to different levels of operator proficiency, and shared practical tips on key aspects such as selecting the appropriate dissection knife based on the lesion’s location and depth, controlling bleeding during submucosal dissection, and maintaining a stable visual field when operating in anatomically challenging areas.
In addition, Specialist Level II, Bui Nhuan Quy, MD, MSc, Head of the Gastroenterology & Hepatology Department at FV Hospital, highlighted the alarming situation of gastric cancer in Vietnam, where most cases are diagnosed at a late stage, greatly limiting treatment effectiveness. Using endoscopic images, Dr Quy demonstrated how early-stage lesions are often small, have atypical appearances, and are easily overlooked without sufficient experience or technical support.

Dr Quy emphasised the importance of training in early diagnostic endoscopy, particularly the use of techniques such as Narrow Band Imaging (NBI) and chromoendoscopy. These advanced methods improve the detection of precancerous and early-stage cancerous lesions, which is critical for enhancing patient outcomes and prognosis.
The programme concluded with the most anticipated segment: hands-on simulation sessions guided directly by Prof Ohya. Using the MIKOTO model, a next-generation endoscopy simulator featuring realistic colon anatomy, lifelike tactile feedback, and AI-based performance recording, analysis, and scoring; participants were able to safely and accurately practise a full range of techniques, from basic to advanced. The simulator also supports unlimited practice attempts, which helps enhance hand-eye coordination as well as force control skills.
In parallel, a hands-on session using pig stomach models was conducted to simulate real clinical scenarios involving actual tissue lesions. This allowed participants to become familiar with tissue elasticity, practise managing minor bleeding, and handle procedural complications, thereby improving confidence and technical competence for real-life applications.
The workshop provided a well-balanced combination of in-depth theoretical knowledge and hands-on simulation, delivering an engaging learning experience for all participants. In addition to mastering ESD techniques and complication management, the programme also created valuable opportunities for knowledge exchange with an international expert, supporting efforts to improve early detection and minimally invasive treatment of gastrointestinal cancers.


 Vi
Vi