During his visit to FV Hospital, Mr C.B., a 45-year-old man from Cambodia, was diagnosed with a rare carotid-cavernous fistula, a condition that can cause severe eye complications and risk vision loss.
Fortunately, he was successfully treated with embolisation, a minimally invasive interventional technique.
Protruding Eye and Near Blindness from Rare Carotid-Cavernous Fistula
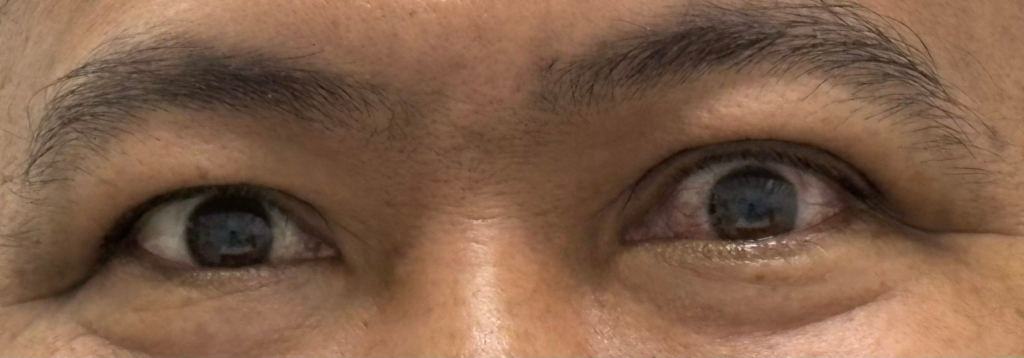
Patient C.B. came to FV Hospital with a red left eye, sharp intermittent pain, and double vision. Having found no relief from previous treatments elsewhere, he decided to travel to Vietnam with the hope that FV’s doctors could save his left eye.
After clinical examination and brain MRI, FV specialists in neurosurgery, interventional neuroradiology, and neurology concluded that this was a carotid-cavernous fistula – a rare condition that affects approximately four people per million.
A carotid-cavernous fistula is an abnormal connection between the carotid artery and the cavernous sinus (a venous sinus). The cavernous sinuses are located behind the eyes, receiving converging venous blood flow from the brain and draining back to the heart via the jugular vein. The arteriovenous shunt causes haemodynamic changes, leading to symptoms such as tinnitus and headache. The ocular venous system is most directly affected, causing manifestations such as proptosis, vision impairment, ophthalmoplegia, and raised intraocular pressure. This abnormal arteriovenous connection can also disrupt cerebral and meningeal circulation, potentially causing severe damage and endangering the patient’s life.

Treatment of Carotid–Cavernous Fistula Using Endovascular Embolisation
The patient was placed under general anaesthesia. Using the Seldinger technique, the interventional radiologist made a small incision in the groin to insert a catheter via the venous route, advancing it to the cavernous sinus, and then navigating along the fistulous carotid artery to the leakage site. At this location, a special embolic glue was injected to seal the fistula. The procedure was carried out over four hours in the Cathlab, supported by Digital Subtraction Angiography (DSA).
However, in this case, the carotid–cavernous fistula was complex, making complete occlusion unachievable with embolisation alone. The interventional radiologists therefore combined the procedure with a carotid compression technique, instructing the patient to compress the carotid artery manually with a finger regularly, eight times a day at home.
The patient’s condition improved rapidly, and he was discharged from hospital. At the 1.5-month follow-up, imaging results were normal, and the patient was completely free of clinical symptoms.

Embolisation: A Sophisticated Technique for Treating Complex Conditions
Embolisation is a minimally invasive procedure offering several advantages, including small incisions, minimal blood loss, no scarring, and a reduced risk of infection or surgical complications. Embolisation is not only used to treat carotid-cavernous fistula but also for a wide range of complex conditions, such as liver tumours, uterine fibroids, prostate tumours, thyroid nodules, and vascular malformations in the brain, arms, legs, abdomen, and nasopharyngeal fibromas.

The procedure was performed by Dr Huynh Huu Danh and the vascular intervention team at FV Hospital. FV is one of the few medical centres to use embolisation in combination with a Digital Subtraction Angiography (DSA) system to treat complex vascular malformations in both adults and children. All procedures are conducted in operating rooms that meet infection control standards in line with international JCI accreditation.
For more information about the embolisation technique, please contact Imaging & Interventional Radiology Department at FV Hospital on (028) 35 11 33 33.

 Vi
Vi 












