What is coronary artery disease?
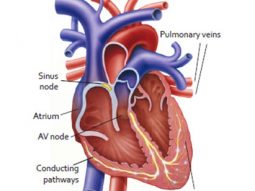
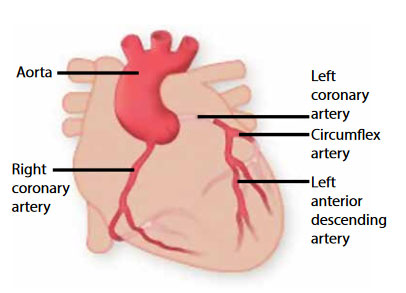
The coronary arteries supply blood to the heart. There are two main arteries, the left and right, which in turn divide into branches.
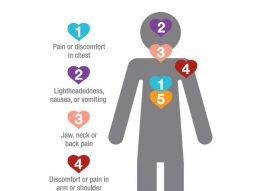
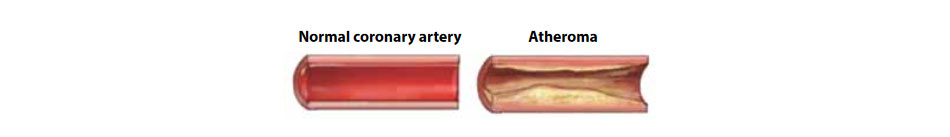
Coronary artery disease is due to the narrowing or blockage of one or more of these arteries by fatty deposits called atheroma. The pain or discomfort, usually in the chest, caused when not enough blood gets to the heart muscles is called angina. A completely blocked coronary artery will cause a heart attack (myocardial infarction).
What are Coronary Angiogram and Percutaneous Coronary Intervention?
A coronary angiogram is an x-ray picture of the coronary arteries using an x-ray “dye” (contrast) to identify narrowed or blocked arteries.
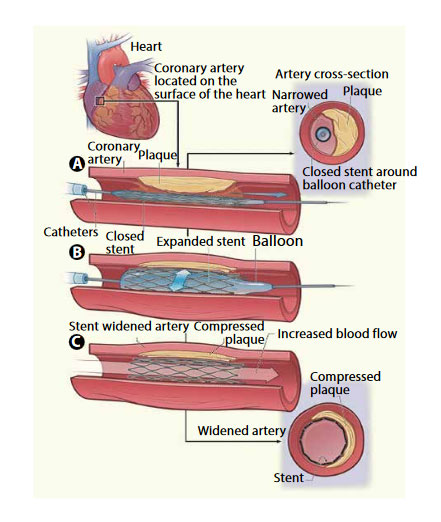
Percutaneous Coronary Intervention (PCI, also called coronary angioplasty or stenting) is a procedure that aims to treat narrowings or blockages in the coronary arteries. During PCI a small balloon is briefly inflated and then deflated in the coronary artery, to stretch the artery and squash the atheroma to the wall of the artery. A stent, which is a small tube of stainless steel mesh, is then inserted into the stretched area of the artery to keep it open and ensure that the blood supply through the artery is maintained. When required, several stents can be inserted.
How is the procedure performed?
The procedure is usually performed through blood vessels in the wrist or groin. You will be given a local anaesthetic to numb the skin around the area where the procedure is performed, sedation is rarely required. A small cut is then made either in the wrist or groin. A sheath (long thin plastic tube) is inserted into the blood vessel. This stays in place during the procedure and acts as a guide, through which the catheters and wires are then inserted and guided up to the heart. This may cause a warm sensation, which is nothing to worry about.
The doctor can see the coronary arteries on the x-ray screen.
While the catheter is in the artery, a number of additional mechanical devices may be used to complete the procedure. These include pressure wires, Rotablator and intravascular ultrasound scanning (IVUS).
If an angioplasty is not required and the test is over the catheter is gently removed. If an angioplasty is decided a fine wire is then passed through the narrowed part of the artery and over this wire a balloon is passed over and inflated in the narrowing. This squashes back the fatty tissue (referred to as atherosclerosis or plaque) responsible for the narrowing.
A stent is then inserted into the narrowed part of the coronary artery. This sits on top of a balloon which inflates and expands the stent. The stent acts as scaffolding to keep the blood vessel open, restoring good blood flow. The balloon is then deflated and removed, leaving the stent in place.
How long does the procedure take?
The procedure usually takes about an hour although this varies depending upon the numbers of narrowings to be treated. Some procedures involve treatment of blocked arteries which can be more complex and might take longer.
Will I have any pain or discomfort?
You will have a local anaesthetic injection to numb the area where the catheter is inserted. The cardiac catheterisation is not painful, but you may feel a slight discomfort like an angina pain. Don’t worry about this (it doesn’t mean anything is wrong) but do tell your doctor. If you have an angioplasty, when the balloon is blown up you may feel a brief chest pain like angina. Don’t worry, but do tell the doctor.
Will the procedure work?
This procedure is usually very successful. If an artery is totally blocked, however, success rates are less. In order to reduce the future risk of developing further narrowings in other parts of the coronary arteries, you will be given advice on the importance of taking the medications prescribed for you and how you can help prevent further heart disease through a lifestyle change with healthy eating and exercise.
What are the risks of this procedure?
Important factors that can affect the risks of this procedure include:
- Age, underlying heart disease, other medical conditions such as diabetes or kidney disease
- How well you are before the procedure, risks are higher if the procedure is carried out in an emergency, after recent heart attacks or when angina is unstable and occurring at rest
Common risks and complications (more than 5%) include:
- Minor bruising at the puncture site.
- After a successful PCI, the coronary artery can become narrowed or blocked again.
- Loss of pulse in the arm after a radial artery procedure (in the wrist)
- Major bruising or swelling at the puncture site.
Uncommon risks and complications (1- 5%) include:
- Abnormal heart rhythm that continues for a long time. This may need an electric shock to correct.
- A heart attack.
- Surgical repair of the groin/arm puncture site or blood vessel.
Rare risks and complications (less than 1%) include:
- The stent may suddenly close within the first month. This can cause angina or heart attack. It may be treated with another PCI or with surgery.
- Emergency heart surgery due to complications with the procedure.
- An allergic reaction to the x-ray dye. This is usually very mild and temporary, such as a skin rash.
- A reaction to the drugs given to prevent blood clotting.
- Loss of kidney function (usually reversible) due to the side effects of the x-ray dye.
- A stroke. This can cause long term disability.
- Rupture of a blood vessel requiring surgical repair and blood transfusion.
- Compartment syndrome
- Death as a result of this procedure is very rare:
- For elective patients: occurs in 1 to 2 patients in 1000 for an angiogram, 1 to 3 in 100 if proceeds to angioplasty
- For emergency patients: occurs in 0.1-0.5% or 1 to 5 in 1000 for an angiogram, 3-10% or 3 to 10 in 100 if proceeds to angioplasty or even more in cardiogenic shock
After the procedure
- Following your procedure you will be hospitalised in the Cardiology ward where staff will monitor your pulse and blood pressure.
- They will check the wound site and circulation in the limb that was used.
- You will be allowed to eat and drink again.
- You may feel a little sore as the local anaesthetic wears off; if you need painkillers, please ask for them.
- When PCI has been scheduled as an elective procedure most patients are able to go home on the morning after the procedure, when performed in emergency the duration of hospitalisation depends on patient’s clinical condition
What happens when I go home?
- Please ask a friend or relative to collect you and accompany you home.
- When the PCI has been carried out as an elective procedure you can usually resume normal activities after 48 hours.
- If the wound in your wrist or leg becomes red, itchy or swollen contact your doctor
- You can usually resume driving 48 hours following the procedure.
- The stent stays in for life. After the procedure, you will be given drugs which reduce your risk of blood clotting and the stent blocking. These are called anti-platelet agents; you will need a combination of two of these drugs, usually aspirin and Clopidogrel (Plavix®).

 Vi
Vi