GASTROSCOPY OVERVIEW
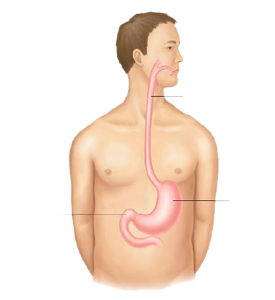
An upper endoscopy (also called “Gastroscopy”) is a procedure used to visually examine your upper digestive system with a tiny camera on the end of a long, flexible tube called “endoscope”. A specialist in diseases of the digestive system (gastro-enterologist) uses endoscopy to diagnose and, sometimes, treat conditions that affect the esophagus, stomach and beginning of the small intestine (duodenum).
The medical term for an upper endoscopy is esophago-gastro-duodenoscopy
There are two types of Gastrocopy:
The classic Gastroscopy during which the endoscope is inserted through the mouth and the Transnasal Gastroscopy (also called “Babyscopy”) during which a thinner endoscope is used and inserted through the nose.
Babyscopy is only used for diagnostic. Ask your doctor which procedure is recommended in your case
WHY IT IS DONE?
Your doctor may recommend a gastroscopy procedure to:
- Investigate symptoms. Endoscopy may help your doctor determine what is causing digestive signs and symptoms, such as nausea, vomiting, abdominal pain, difficulty swallowing and gastrointestinal bleeding.
- Diagnose. Your doctor may use endoscopy to collect tissue samples (biopsy) to test for diseases and conditions such as anemia, bleeding, inflammation, diarrhea or cancers of the digestive system
- Treat. Your doctor can pass special tools through the endoscope to treat problems in your digestive system, such as burning a bleeding vessel to stop bleeding, widening a narrow esophagus, clipping off a polyp or removing a foreign object. Treatment procedures always require a classic gastroscopy procedure (as the endoscope used for Babyscopy is too thin for the necessary instruments.
ENDOSCOPY PREPARATION
Prior to the endoscopy, your doctor will review your medical and surgical history, including current medications. Tell your doctor about all the medications and supplements you are taking before your endoscopy
You will be asked to sign a consent form that says you understand the risks of gastroscopy and agree to have the test done. Talk to your doctor about any concerns you have regarding the need for the test, its risks, how it will be done, or what the results will mean
Your doctor will give you specific instructions to prepare for your gastroscopy. In some cases your doctor may ask that you:
- Fast before the gastroscopy. You may be asked to stop drinking and eating four to eight hours before your gastroscopy to ensure your stomach is empty for the procedure.
- Stop taking certain medications. You may be asked to stop taking certain blood-thinning medications in the days before your endoscopy. Blood thinners may increase your risk of bleeding if certain procedures are performed during endoscopy. If you have chronic conditions, such as diabetes, heart disease or high blood pressure, your doctor will give you specific instructions regarding your medications.
Sedation
Classic gastroscopy without sedation is not recommended because of bad tolerance. Patients undergoing a gastroscopy will receive a sedative to relax them and make them more comfortable during the procedure. They will be admitted in the Day Ward and the gastroscopy will be performed in the dedicated endoscopy unit. If you are sedated during the procedure, plan ahead for your recovery while the sedative wears off. You may feel mentally alert, but your memory, reaction times and judgment may be impaired. Find someone to drive you home. You may also need to take the day off from work. Don’t make any important personal or financial decisions for 24 hours
Babyscopy often does not require sedation and can be done in a dedicated room located in the outpatient department
THE ENDOSCOPY PROCEDURE
- During a gastroscopy procedure, you will be asked to lie down on a table on your back or on your side.
- Monitors often will be attached to your body to allow your health care team to monitor your breathing, blood pressure and heart rate. You may receive a sedative medication through a vein in your forearm. This medication helps you relax during the endoscopy.
- Classic gastroscopy:
- Your doctor sprays an anaesthetic in your mouth to numb your throat in preparation for the insertion of the endoscope. You are asked to wear a plastic mouth guard to hold your mouth open. Then the endoscope is inserted in your mouth. Your doctor may ask you to swallow as the scope passes down your throat. You may feel some pressure in your throat, but you should not feel pain.
- You cannot talk after the endoscope passes down your throat, though you can make noises. The endoscope does not interfere with your breathing.

- Transnasal Gastroscopy:
- Your doctor sprays and applies an anaesthetic into your nostril to numb your nose. An anaesthetic may be sprayed through your mouth to numb your throat as well.
- The endoscope covered with anaesthetic (lidocaine) jelly is inserted into your nostril then through the back of your mouth and you are asked to swallow. You are able to speak during the procedure if you need to.
- As your doctor passes the endoscope down your esophagus, a tiny camera at the tip transmits images to a video monitor in the exam room. Your doctor watches this monitor to look for abnormalities in your upper digestive tract. If abnormalities are found in your digestive tract, your doctor may record images for later examination.
- Gentle air pressure may be fed into your esophagus to inflate your digestive tract so the endoscope can move freely and the folds of your digestive tract are more easily examined. The air can create a feeling of pressure or fullness.
- Your doctor may pass special surgical tools through the endoscope for example to collect a tissue sample (biopsy) or perform specific treatments (such as dilatation, removal of polyps, treatment of bleeding), depending upon what is found during the examination
- When your doctor has finished the exam, the endoscope is slowly retracted through your mouth. Endoscopy typically takes five to 20 minutes, depending on your situation.
RECOVERY FROM ENDOSCOPY
You will be taken to a recovery area to sit or lie quietly after your endoscopy. You may stay for an hour or so. This allows your health care team to monitor you as some time is needed for the sedative to wear off. Recovery is faster after a transnasal gastroscopy than after a classic gastroscopy.
Elderly patients undergoing gastroscopy are advised to have a support person who transports them home and stays with them for several hours.
Once you are at home, you may experience some mildly uncomfortable signs and symptoms after endoscopy, such as:
- Bloating and gas
- Cramping
- Sore throat
- Sore nose (if you underwernt a transnasal gastroscopy)
These signs and symptoms will improve with time. If you are concerned or quite uncomfortable, call your doctor.
Take it easy for the rest of the day after your endoscopy. You may feel alert, but your reaction times and judgment are delayed after receiving a sedative
Most patients are able to eat shortly after the examination.
GASTROSCOPY COMPLICATIONS
Gastroscopy is a very safe procedure. However gastroscopy carries a very small risk of complications. Rare complications include:
- Aspiration (inhaling) of food or fluids into the lungs, the risk of which is minimized by not eating or drinking for the recommended period of time before the examination.
- There is a very small risk of adverse reaction to one of the drugs used in the procedure. For this reason please let your doctor know all the medicines you are taking and any allergies you have to drugs or other substances.
- Bleeding. Your risk of bleeding complications after endoscopy is increased if the procedure involves removing a piece of tissue for testing (biopsy) or treating a digestive system problem. In rare cases, such bleeding may require a blood transfusion.
- Infection. Most endoscopies consist of an examination and biopsy, and risk of infection is low. The risk of infection increases when additional procedures are performed as part of your endoscopy. Most infections are minor and can be treated with antibiotics. Your doctor may give you preventive antibiotics before your procedure if you are at higher risk of infection.
- Tearing of the gastrointestinal tract. A tear in your esophagus or another part of your upper digestive tract may require hospitalization, and sometimes surgery to repair it. The risk of this complication is very low — it occurs in an estimated 3 to 5 of every 10,000 diagnostic upper endoscopies.
Signs and symptoms that could indicate a complication include
- Fever
- Chest pain
- Shortness of breath
- Black or very dark colored stool
- Difficulty swallowing
- Severe or persistent abdominal pain
- Vomiting
Call your doctor immediately or go to FV emergency department if you experience any of these signs or symptoms.
RESULTS OF THE PROCEDURE
The doctor can describe the result of the gastroscopy as soon as it is over.
If a sample of tissue (biopsy) was collected during the gastroscopy, it will be sent to a pathology lab, where it is looked at under a microscope for diseases. The results of tests sent to a lab will be available within one to two weeks. Ask your doctor when you can expect the results of your endoscopy.
A follow-up appointment or phone call is usually scheduled after a biopsy to discuss the results of the tissue analysis
This brochure is not intended to take the place of a consultation with your doctor about your gastroscopy. If you have questions about the examination or subsequent follow-up, please discuss them with your doctor before or after the examination.

 Vi
Vi 












