Breast cancer is one of the most common cancers around the world and is the leading cause of cancer-related deaths in women. Many women diagnosed with breast cancer think that they must undergo mastectomy as they believe that the complete removal of all possible cancer sources may help to ensure that cancer doesn’t recur. However, in many cases, breast cancer patients have several treatment options to cure them of cancer while preserving their natural beauty.
At the end of 2013, Ms. T., a 55-year-old patient, was admitted to FV Hospital for breast cancer treatment after a malignant 1cm tumour was found in her left breast. After a multidisciplinary consultation, the patient was recommended to undergo tumorectomy (conservative breast surgery) with the removal of sentinel lymph nodes without chemotherapy. Ms. T then received adjuvant radiotherapy, which she tolerated very well with no complications. “The breast radiotherapy decreases the risk of breast cancer relapse by 70 per cent,” explains Dr. Bertrand Farnault, Head of Hy Vong Cancer Care Centre.
Surgical treatment options for breast cancer
Ms. T is one in thousands of breast cancer patients being successfully treated at Hy Vong Cancer Care Centre, FV Hospital.

Normally, cancer patients experience several stages of the disease and different treatment options for each stage. When treating breast cancer, surgery is often the first step to be taken. There are two surgery options for breast cancer that are proven to have equivalent treatment outcomes.
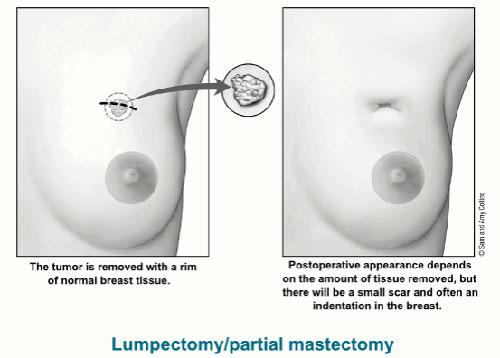
A lumpectomy implies the complete removal of the malignant breast tumour with a concentric margin of surrounding healthy tissue while preserving the cosmetic appearance of the breast.
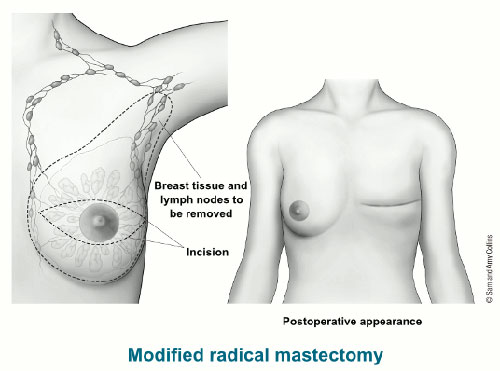
A mastectomy implies the complete removal of the whole breast and lymph nodes.
Breast conservation treatment or lumpectomy with support of radiotherapy is a very well established alternative to a mastectomy. Many studies have shown that this combined treatment has equivalent survival rates and range of local control as mastectomy.
As these two surgical treatment options have near equal efficiency, the selection of either lumpectomy or mastectomy depends largely on the specific cancer case and personal preference of the patient.
In cases of larger tumours or multiple tumours (i.e. multiple independent deposits of cancer cells spread throughout the breast), mastectomy is the only option. The disadvantage of a mastectomy is the loss of the breast. This may cause a negative emotional and physical impact on the patient as patients undergoing mastectomy not only suffer physical pain but often also lose their self-esteem as they feel that without their breasts, they have lost some of their femininity.
On a positive note, breast reconstruction techniques continue to improve. This can give patient a reconstructed breast with excellent cosmetic appearances in most cases; however the recuperation time is longer that for lumpectomy and requires more energy from the patient to recover fully.
If breast cancer is detected in the early stages with smaller tumours, the best option for patients is surgery to preserve the breasts. It’s the reason why breast screening with mammography every two years is very important for women from 40 years old. This treatment option has a more positive psychological impact for patients as the breast is preserved but radiotherapy following surgery is required.
Selecting the best treatment option
Oncologists and surgeons at Hy Vong Cancer Care Centre, FV Hospital dedicate time to informing breast cancer patients about their case and helping them to make an intelligent decision on which treatment option is the best for them. When a decision between a mastectomy and a lumpectomy has to be made by the patient, it is a very personal one. Many women feel strongly about one option over another. FV physicians always respect the patient’s decision, as long as the patient is well informed about the medical facts and their options.
However, when it comes to surgical treatments for breast cancer, many patients believe erroneously that mastectomy is better than tumorectomy. They worry that cancer could spread to surrounding healthy tissues from any residual cancer cells if only the tumours are removed. These patients choose mastectomy as they think that mastectomy can completely remove every cancer cell.
This thinking is not necessarily wrong, but patients should have a good understanding of preservative breast surgery and how they can benefit from this treatment.
- The main advantage of a lumpectomy is simply preservation of the breast. For many women, choosing to undergo lumpectomy could have a more positive image on their psychological state and body image.
- Breasts are often perceived by women as an important part of their identity; it makes sense that most patients would prefer to preserve their breasts if at all possible. No matter what your age, breast preservation is a strong option as it does not endanger your overall health and chance of a full recovery.
- Lumpectomy takes a shorter time to perform as it is a less extensive surgery than mastectomy. Breast conservation treatment also reduces the risk of post-surgical side effects and shortens the recuperation time.
- Radiotherapy following breast conservation surgery decreases the risk of breast cancer relapse by around 70 per cent. This treatment is well tolerated by most patients and shown to be extremely safe.
- At FV Hospital, in some selected cases, neoadjuvant therapy (preoperative treatment), such as chemotherapy can change a patient’s surgical options. Neoadjuvant therapy may shrink a tumour enough so that a lumpectomy becomes an option instead of a mastectomy.
Once again, whether a lumpectomy or mastectomy is recommended by your surgeon or is your individual preference, it is important to note that both are equally effective treatments for cancer. As a patient, you should choose the option which is better for your specific cancer case and with which you are most comfortable.
Dr. Bertrand Farnault, Head of Hy Vong Cancer Care Centre, says: “When I explain to patients that they have more than one option, many of them ask me ‘What would you do if it was your family members?’ I always say, I’d explain the specifics of the case to patients in the same way I do for my family members and let them make their decision regarding the best treatment for them. For those cases in which the scientific information shows patients can make their own choice regarding treatment, I feel confident to go either way. It is basically a matter of which option the patient feels most comfortable with.”

 Vi
Vi