Colorectal resection
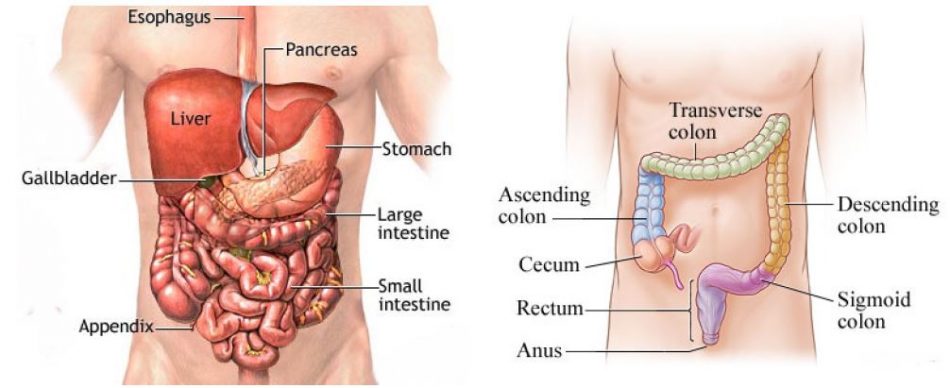
WHAT IS THE LARGE INTESTINE?
The large intestine (or large bowel) is the lower part of the digestive system where waste products from the food you eat are collected and processed into faeces.
The large intestine is about 1.5 m long and consists of the caecum, appendix, colon and rectum – which are distributed in the abdominal cavity.
WHAT DOES IT DO?
The large intestine performs the following functions:
- Reabsorbs water and maintains the fluid balance of the body
- Absorbs certain vitamins
- Processes undigested material (fibre)
- Stores waste before it is eliminated.
WHAT IS COLORECTAL RESECTION? AND WHY IS IT NECESSARY?
A colorectal resection is a surgery to remove a section or the whole of the large intestine. It is done to remove injured or diseased parts of the colon.
This surgery is performed to treat a variety of conditions, including the following:
- Colorectal cancer
- Diverticular disease – small pouches form in the wall of the colon
- Inflammatory intestinal diseases colitis,Crohn’s disease
- Large bowel obstruction
- Trauma to the intestine
- Precancerous polyps, especially those seen in familial polyposis
- A hole in the bowel wall or dead piece of bowel
- Bleeding from the colon
For colon cancer, the goal is to remove all of the cancer. If you have a precancerous condition, then you may have prevented the development of cancer. If you had surgery due to other conditions, a successful operation will alleviate or improve your symptoms.
During a colon resection, the diseased part of the bowel is removed and the two healthy sections of the colon are reattached. If an anastomosis is not possible because of the extent of the disease or its location, the surgeon creates a colostomy. A temporary colostomy is made when the colon needs longer to heal after surgery and the anastomosis is performed later.
HOW IS IT PERFORMED?
Colorectal resection is performed under general anesthesia.
There are two types of colon resection: open surgery and laparoscopic surgery. The type of procedure performed depends on the diagnosis and the individual patient.
- Open colorectal resection – where the surgeon makes a large midline incision in your abdomen in order to remove a section or the whole of the large intestine.
- Laparoscopic or ‘keyhole’ colorectal resection – where the surgeon makes a number of smaller cuts in your abdomen, before using a special telescope and small surgical instruments to remove a section or the whole of the large intestine. A slightly larger incision is usually made to remove the diseased section of colon from the body.
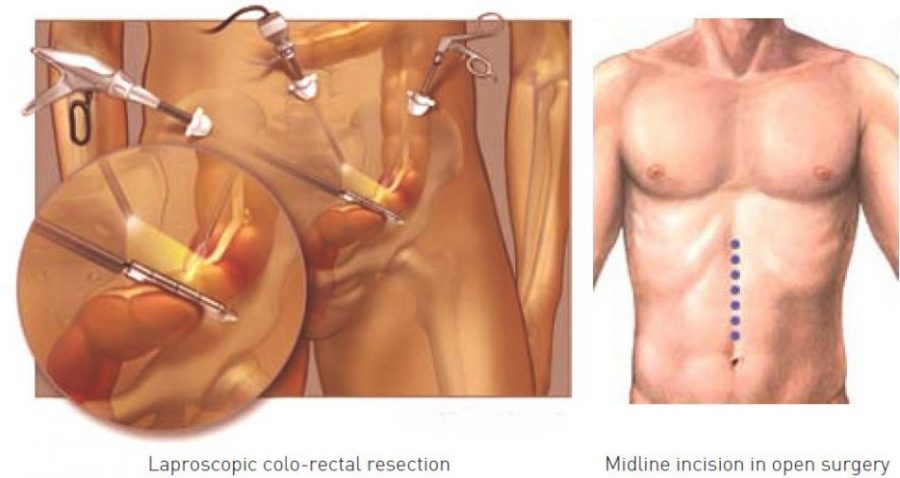
Laparoscopic colorectal surgery is a new technique that is rapidly gaining popularity. Advantages of laparoscopy include the following:
- Colon function normalizes faster
- Faster recovery time and shorter hospitalization
- Less postoperative pain
- Quicker return to normal activities
- Smaller scar
According to the site of the diseased large intestine, there’re many kinds of operation:
- Right hemicolectomy and left hemicolectomy refer to the resection of the ascending colon (right) and the descending colon (left), respectively and 1/3 of the transverse colon. When 2/3 of the transverse colon is also resected, it may be referred to as an extended hemicolectomy
- Transverse colectomy is also possible, though uncommon.
- Sigmoidectomy is a resection of the sigmoid colon, sometimes including part or all of the rectum (proctosigmoidectomy). When a sigmoidectomy is followed by terminal colostomy and closure of the rectal stump, it is called a Hartmann operation; this is usually done out of impossibility to perform a “double-barrel” or Mikulicz colostomy, which is preferred because it makes “takedown” (reoperation to restore normal intestinal continuity by means of an anastomosis) considerably easier.
- When the entire colon is removed, this is called a total colectomy. If the rectum is also removed, it is a total proctocolectomy.
- When the entire rectum and part of sigmoid colon is removed by abdominal and perineal approach, this is called a Miles’ procedure.
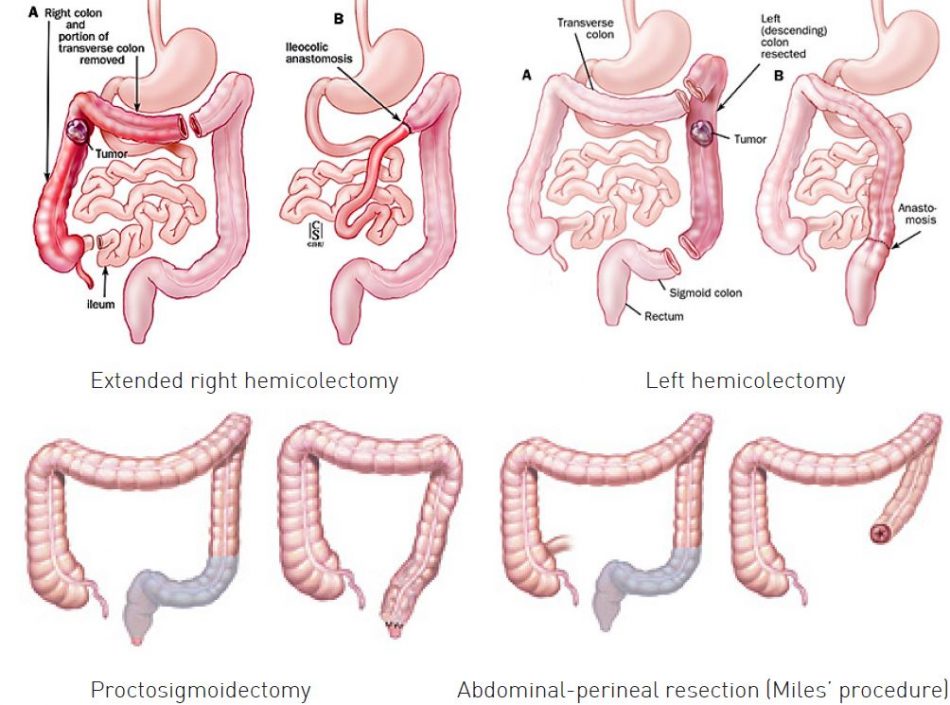
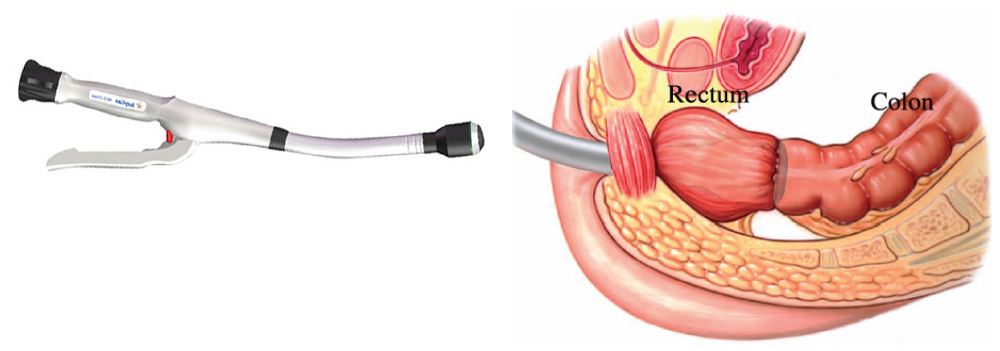
If recto-sigmoidectomy is performed, circular stapler is used to make colorectal anastomosis.
PREPARATION BEFORE OPERATION
You will need to attend a pre-anesthesia appointment a few days before surgery. The appointment may involve having some blood tests and a general health check depending on your age and medical condition to make sure that you are fit for surgery.
It is recommended that you shower the night before and morning of the operation with Betadine scrub (an antiseptic solution).
The colon contains bacteria and waste products that can cause infection if they leak into the abdomen during surgery. Therefore, a number of precautions are taken to reduce this risk.
First, oral antibiotics may be prescribed several days before the operation. Second, the colon is emptied as much as possible to reduce the risk for infection during surgery.
Generally, 2 or 3 days prior to surgery, a soft or semi liquid diet (only foods that are quickly and easily digested) is ordered. Sometimes, only clear liquids (e.g., fruit juice, clear broth,…) are permitted. All patients go on a clear liquid diet 24 hours before surgery and nothing may be taken by mouth after midnight.
On the day before surgery, patients are asked to drink a laxative solution. Because the solution can cause severe diarrhea, some facilities admit patients for this and give them intravenous fluids to avoid dehydration.
If the patient is unable to comply with this regimen, it is necessary to inform the surgeon right away. It may be unsafe to perform the surgery and the procedure may be postponed.
RISKS OF COLORECTAL RESECTION
Like any surgical procedure, a colorectal resection carries risks of complications. These complications may include complication from anesthesia, pneumonia, urinary tract infection, heart attack…
Some possible surgical complications of colorectal resection include:
- Damage to other organs or structures
- Bleeding
- Infection
- Leakage from the anastomosis
- Intra-abdominal abscess (a pus-filled swelling),
- Infection of the membrane that lines the abdominal cavity (peritonitis),
- Hernia forming at the incision site
- Anastomosis stenosis
- Intestinal obstruction due to development of scar tissue
Some complications will require further surgery.
RECOVERY AFTER SURGERY
After colorectal resection, the patient is taken to the recovery room (RR) and is closely monitored by the nursing staff until the anesthesia wears off. When vital signs are stable and the patient is awake and coherent, he or she is transferred to the surgical ward or sometimes to the intensive care unit (ICU) when needed.
On the day after surgery, most patients can get out of bed and move around. It is important to get up as soon as possible, because physical activity stimulates bowel function and helps blood circulation return to normal.
Until you are able to eat and drink normally, you will be fed intravenously (through a tube inserted directly into a vein). Most people are able to resume a light diet between 4-5 days after having a colorectal resection.
You will need to take painkillers for a few days. You should tell your treatment team if the painkillers that you are taking aren’t working because alternative painkillers are available. Antibiotics may also be given postoperatively. This depends on a number of factors, including the original diagnosis.
Following a colorectal resection, you will probably be able to return home within 1-2 weeks after having the operation.
Normal activity for all patients generally resumes within 1 to 3 weeks, but it takes much longer for the body to heal completely. So, patients must avoid strenuous exertion and heavy lifting for 4 to 6 weeks.

 Vi
Vi