FV Hospital has successfully removed a brain tumour measuring over 6 cm in diameter by combining vascular embolization, the advanced Navigation eurosurgical guidance system, and ultrasonic tumour dissection technology. The tumour was meticulously dissected and entirely removed within four hours, without damaging surrounding brain tissue and with minimal blood loss. Remarkably, the patient began to recover just two hours after surgery.


Stroke Screening Reveals Large Brain Tumour Compressing Brain Tissue
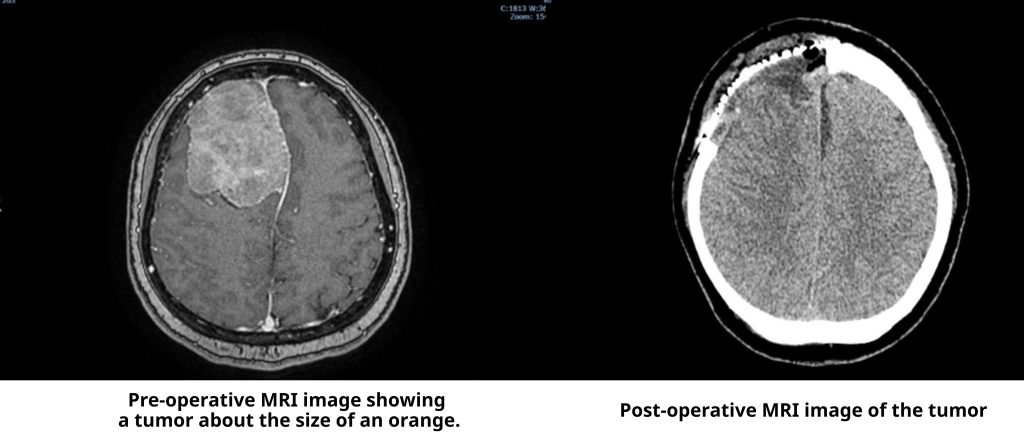
Ms Trinh Nhat Khanh, a 45-year-old martial arts instructor living in Ho Chi Minh City, occasionally experienced mild headaches and decided to undergo a stroke screening at FV Hospital. An MRI scan unexpectedly revealed a large meningioma measuring over 6 cm in diameter — approximately the size of an orange — compressing nearly a quarter of her brain.
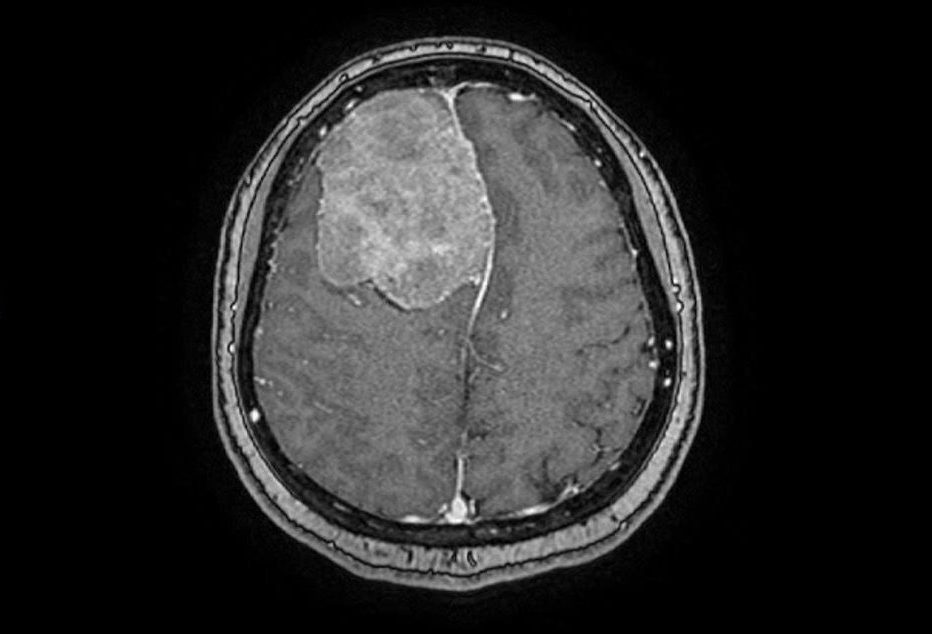
“The tumour had developed over a long period, allowing the skull to adapt to it, which made it difficult to detect. Although the patient experienced only occasional headaches and her higher brain functions remained unaffected, surgery was urgently needed. If the tumour grew any larger, it could trigger serious complications such as seizures or even become life-threatening,” explained Dr Tran Luong Anh, Specialist Level II and Head of Neurosurgery and Spine Surgery at FV Hospital.
Following a multidisciplinary consultation between Imaging & Interventional Radiology Department and the Neurosurgery & Spine Surgery Department, the medical team identified two major challenges to a successful surgery. First, the tumour’s large and firm structure posed a risk of damaging surrounding brain tissue during removal. Second, it was being supplied by numerous blood vessels, increasing the risk of significant blood loss during the procedure.
Combining Vascular Intervention and Navigation Technology to Safely Remove the Tumour While Preserving Brain Tissue
To minimise intraoperative blood loss and protect vital vessels, Dr Luong Anh consulted with Dr Huynh Huu Danh, Specialist Level I and interventional radiologist from the Imaging and Interventional Radiology Department – Interventional Radiology Unit, to perform a pre-operative embolisation. This procedure was carried out one day before the surgery to block the tumour’s blood supply. According to Dr Danh, embolisation is a minimally invasive technique commonly used to treat certain brain conditions, including arteriovenous malformations, brain aneurysms, carotid-cavernous fistulas, and dural arteriovenous fistulas.

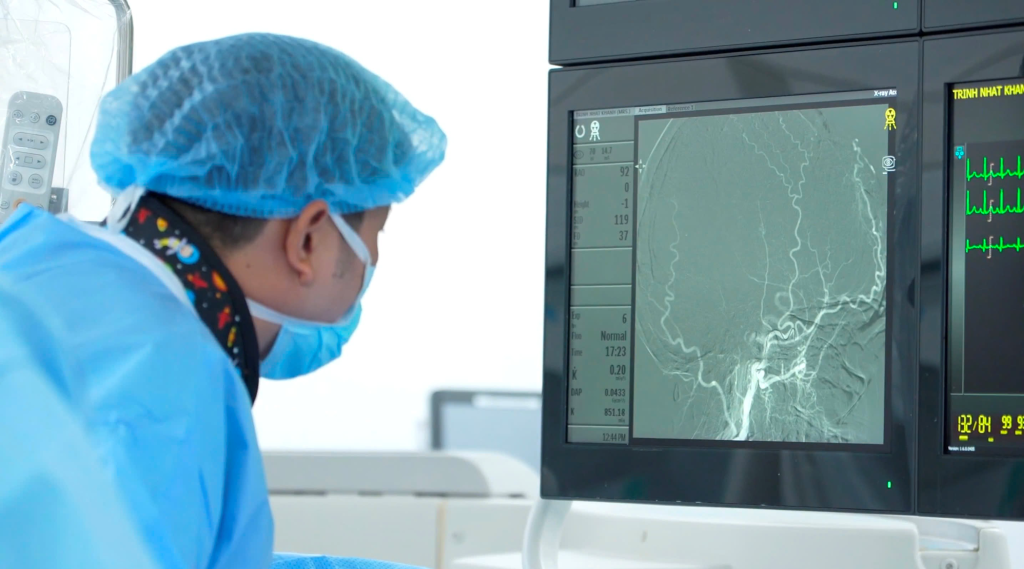
Dr Huynh Huu Danh performed the embolisation procedure, which lasted around 30 minutes and successfully blocked approximately 90% of the tumour’s blood supply.
The following day, the surgery led by Dr Tran Luong Anh was performed with the support from the Navigation System, which accurately identified the tumour boundaries and optimised the incision path, avoiding cuts that were too large or too small. This helped significantly reduce the surgery time and minimise potential complications. The system also aided in identifying and preserving critical blood vessels near to the tumour.
The surgery was further supported by an ultrasonic aspirator, which helped overcome the challenge of the tumour’s firmness. “For large, firm tumours like this one, manual removal can risk damaging surrounding brain tissue. The ultrasonic aspirator enables us to remove the tumour with minimal manipulation, reducing impact on brain tissue and protecting nearby vessels,” explained Dr Luong Anh.

Through a single, carefully planned incision, the surgical team meticulously dissected and successfully removed the tumour during a four-hour operation without damaging surrounding brain tissue. Thanks to the pre-operative collaboration with the interventional neuroradiologist, who embolised the tumour’s blood supply, intraoperative blood loss was significantly reduced, and the surgery time was shortened. Remarkably, the patient began to recover just two hours after the procedure.
“Normally, with tumours of this size, blood loss during surgery can range from 700 to 1,000 ml. Thanks to the embolisation technique performed prior to surgery, blood loss was reduced to only around 200-250 ml,” Dr Luong Anh shared.

Minimising blood loss during surgery is critically important, as it provides ideal conditions for surgeons to dissect and remove the tumour with greater precision. Surgeons can also avoid repeated cauterisation manoeuvres, reducing trauma to the surrounding brain tissue. This also helps to eliminate the risks associated with blood transfusions.
“Blood transfusions always carry certain risks, such as allergic reactions or the potential transmission of blood-borne diseases. Significant blood loss can also disrupt the patient’s clotting system, requiring us to administer clotting factors. By reducing blood loss, we were able to avoid transfusions entirely. This not only lowers the patient’s risk but also reduces treatment costs,” explained Dr Luong Anh.
“The surgery was a success, with no unexpected complications”
After regaining consciousness following the major brain surgery, Ms Trinh Nhat Khanh made a remarkable recovery. Although she was expected to stay in the ICU for two nights, she was strong enough to be moved to a general ward after just one night. Four days post-surgery, her physical condition had returned to about 90 percent of normal, and her spirits were high. She greeted the doctors and nurses with a beaming smile, full of energy.
“Perhaps it’s thanks to the excellent postoperative care at FV that I didn’t feel any pain after the surgery,” shared Ms Trinh Nhat Khanh.
Sixteen years ago, Ms Khanh chose FV Hospital as the place to welcome her first daughter into the world. Since then, FV has remained her family’s healthcare provider. “I go to FV for everything, from check-ups to treatment. So when this illness appeared, I naturally chose to have the surgery here. I have many friends who are professors and highly skilled doctors at major hospitals in Ho Chi Minh City, yet I still trust FV,” she said.
While her family was shocked by the discovery of a large brain tumour, Ms Khanh remained optimistic and confident about the outcome of the surgery. After hearing the treatment plan, she gave her full consent, placing her trust in the expertise of FV’s doctors. “Dr Luong Anh is highly skilled. Thanks to his talent, my surgery involved very little bleeding, and I was able to recover quickly,” she said with deep appreciation.
According to Dr Luong Anh, the surgery proceeded exactly as planned, with no unexpected complications, thanks to meticulous preparation. The operation was carefully coordinated through a multidisciplinary approach involving not only the surgical and anaesthesia teams, but also the nursing staff and specialists from departments such as Cardiology, Respiratory Medicine, Endocrinology, and most notably, the Interventional Radiology Unit.

“Before every surgery, we always anticipate all possible complications. For example, we ensure there is a supply of blood ready in case of bleeding. The post-operative recovery plan is thoroughly discussed with the anaesthesiologist, including preparations for possible seizures or other irregularities during and after the surgery. We also coordinate with follow-up units, for instance, if the pathology results had shown a malignant tumour, we would have consulted the Hope Cancer Centre to develop a suitable treatment plan, such as chemotherapy or radiotherapy. Fortunately, this was a benign tumour, and the patient will soon return to her normal life, as we were able to preserve nearly all of her brain tissue during the operation,” said Dr Luong Anh.
Dr Tran Luong Anh played a pivotal role in the success of the surgery. He is one of the few specialists in Vietnam with expertise in both brain and spinal neurosurgery. With extensive experience in managing complex cases, he consistently collaborates closely with doctors from various specialties to deliver the best treatment outcomes for patients.
To book a consultation with Dr Tran Luong Anh, Specialist Level II, for neurological or spinal conditions, please contact Neurosurgery & Spine Surgery Department, FV Hospital: (028) 35 11 33 33.

 Vi
Vi 












