What is diabetic vascular disease?
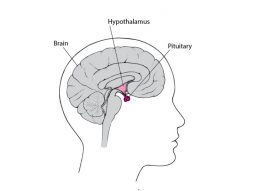
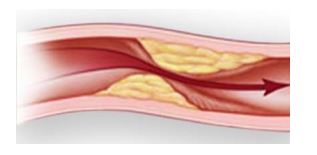
Diabetic vascular disease refers to the development of blockages in the arteries, sometimes called “hardening of the arteries”, throughout the body because of diabetes. If you have diabetes, it means that too much glucose (blood sugar) is in your bloodstream because of your body’s inability to either produce insulin or to use insulin efficiently. Insulin is a hormone that you need to transport glucose from the bloodstream into your cells where it is used to produce energy.
You may also develop several vascular diseases that have been linked to diabetes. One of these is retinopathy, which is the abnormal growth of blood vessels in your retina, which is part of your eye. Another condition linked to diabetes is a kidney disease called nephropathy. If you have diabetes, you are also more prone to hardening of the arteries,
high cholesterol, high blood pressure, and coronary heart disease. You may also develop neuropathy, a condition of the nerves themselves that causes a loss of protective sensation in the toes or feet.
Controlling your blood sugar is the best way to slow or prevent these vascular problems. If you do not manage your diabetes or maintain healthy habits, you could develop serious health conditions, including blindness, severe kidney disease, stroke, heart attack, or sores in your feet. Eventually, if you develop dead tissue, which is known as gangrene, it could lead to infection and ultimately to amputation.
What are the symptoms?
If you have diabetes-related vascular problems, you may have the following symptoms:
- Blurry vision
- Floating spots in your vision called floaters
- Swelling of your face or limbs or unexpected weight gain
- Foamy looking urine
- Foot sores
- Loss of feeling or a burning feeling in your hands or feet
- Pain in your legs when walking
- High blood pressure
- Chest pain
What causes diabetic vascular disease?
If you have diabetes, it may increase the chances for the development of several vascular diseases. Your risk of vascular disease increases with the length of time you have had diabetes. You also increase your risk of developing diabetic vascular disease if you have high blood pressure, if you smoke, don’t exercise, are overweight, or eat a high-fat diet.
What tests will I need?
First your physician asks you questions about your general health, medical history, and symptoms. In addition, your physician conducts a physical exam. Together these are known as a patient history and exam. To confirm a diagnosis of diabetes, your physician will perform a blood test to measure your glucose level. Because diabetic vascular disease can affect many different locations in your body, such as your blood vessels, eyes, and kidneys, its diagnosis and treatment will often involve the collaborative approach of a variety of physicians such as vascular surgeons, ophthalmologists, nephrologists, and endocrinologists.

If your physician suspects diabetic kidney disease, he or she may order a urine test to check for high levels of a certain protein called albumin. Your physician may also perform a kidney biopsy to confirm the diagnosis or determine the severity of the disease. Many of these studies will be evaluated under the guidance of a physician that specializes in kidney disease, known as a nephrologist.
If your physician or ophthalmologist suspects diabetic retinopathy, he or she may perform ophthalmoscopy or a fluorescein angiogram. For ophthalmoscopy, your physician evaluates the blood vessels in your retinas with a hand-held device called an ophthalmoscope. In a fluorescein angiography, an ophthalmologist uses a dye called fluorescein to visualize the vessels in your eye and photographs your eye with a special camera.
Other tests that are often used to diagnose diabetic vascular disease involving the legs include exercise treadmill testing, an ankle/brachial index (ABI), and duplex ultrasound. For the treadmill test, sometimes also called ECG stress testing, you walk or run on a treadmill while your physician measures your heart’s electrical activity. The test can help detect poor blood flow.
For the ABI, your physician measures your blood pressure in your ankle and in your arm, and then compares the two numbers to determine your ABI. Normally, the blood pressures in your ankle and arm should be about equal. But if your ankle pressure is half your arm pressure (or lower), your leg arteries are probably narrowed somewhere along their course.
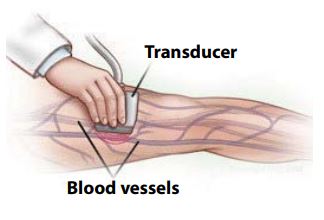
Duplex ultrasound uses sound waves higher than human hearing can detect and are reflected by your arteries and blood cells. Your physician uses Duplex ultrasound to measure the speed of blood flow and to see the structure of your leg vessels.
Your physician may also perform blood tests to measure your cholesterol level as well as the levels of other blood fats (lipids).
How is diabetic vascular disease treated?
Diet and medication
Maintaining healthy blood sugar levels, controlling high blood pressure, and controlling lipid levels through diet and medications all play an important part in diabetic vascular disease treatment. Your physician can provide advice regarding the optimum diet for your particular needs.
Insulin or glucose-lowering medications help control blood sugar levels. Medications to lower blood pressure include angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, calcium channel blockers, and diuretics. Cholesterol lowering medications include statins, which reduce the amount of cholesterol in your blood.
To help keep your blood from clotting, your physician may prescribe antiplatelet medications, such as aspirin and clopidogrel (Plavix).
Retinopathy treatment
If you have retinopathy, your physician may recommend laser surgery, in which a surgeon removes the abnormal blood vessel growth that is affecting your vision.
PAD treatment
When peripheral arterial disease (PAD) causes sores to develop on your feet, your physician will use dressings and sometimes antibiotics to help heal the sores before they become too extensive or deep. He or she will determine if enough blood is reaching the sores to allow them to heal. It is important to treat the sores promptly because if the sores become so bad that the tissue of your foot dies, or the deep tissues or bones become infected, your surgeon may need to partially or completely amputate your foot or leg.
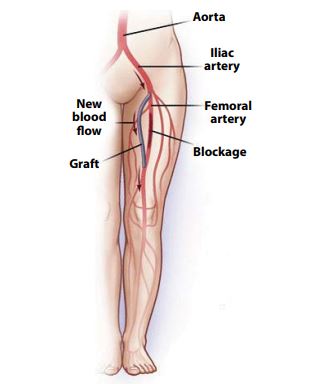
To restore circulation to your leg and avoid amputation, your surgeon may need to perform a procedure such as angioplasty or bypass surgery. Bypass surgery creates a detour around any narrowed or blocked sections of your artery. To perform a bypass, your surgeon connects an artificial or transplanted blood vessel to the blocked artery to help blood flow around the blockage in your affected leg. The blood then flows through the new vessel, bypassing the blocked part of the artery. Sometimes the blockage itself can be removed with a procedure called an endarterectomy.
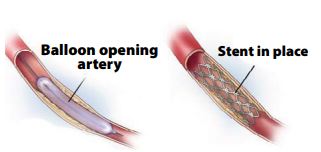
Another treatment option for PAD is a minimally invasive procedure called angioplasty and stenting. In an angioplasty, a long, thin, flexible tube called a catheter is inserted through a puncture, or sometimes through a tiny incision, into an artery in your leg above the narrowed section and is guided through your arteries to the blocked area. Once there, a special balloon attached to the catheter is inflated and deflated, sometimes several times. The balloon pushes the plaque in your artery against your artery walls, widening the vessel. If needed, a tiny mesh-metal tube called a stent may then be placed into the narrowed area of your artery to keep it open. The stent remains permanently in your artery. After successful angioplasty, blood flows more freely through your artery. Your general health, as well as the location and extent of the blockage, determine what procedure is likely to work best in your particular situation.
What can I do to stay healthy?
There are many lifestyle changes that you can make to improve your health and stay healthy. They include quitting smoking, eating a low-fat diet, maintaining a healthy weight, and exercising regularly. You should also monitor your blood glucose level several times per day, as directed by your physician. To prevent foot sores, you should examine your feet daily. If you have a tendency toward dry skin, use a lanolin-based moisturizing cream to prevent callus buildup and cracking. Always protect your feet from injury and keep them dry.

 Vi
Vi