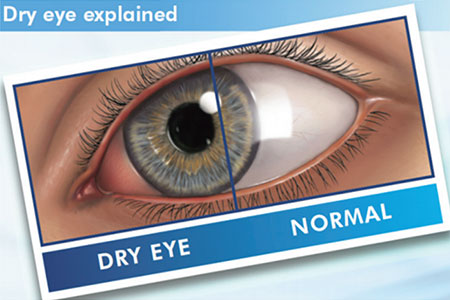
Dry eye, also called keratoconjunctivitis sicca, is dryness of the membranes surrounding the eye. It happens when there are not enough healthy, natural tears in the eyes. The eyes must remain moist at all times. A small amount of tears is constantly produced by the tear glands (lacrimal glands). These glands are located under the outside part of the upper eyelids.
CAUSES
This condition may be caused by:
- Not making enough tears (aqueous tear-deficient dry eyes);
- Tears evaporating from the eye too quickly (evaporative dry eyes). This is when there is an abnormality in the quality of your tears. This abnormality causes your tears to evaporate so quickly that the eye cannot be kept moist.
Dryness of the eyes can be a symptom of a variety of conditions, such as rheumatoid arthritis, lupus, or Sjögren syndrome. Dry eye may be mild to severe.
RISK FACTORS
This condition is more likely to happen because of the following:
- Laser eye surgery may cause temporary dry eye symptoms;
- Prolonged periods of screen time encourage insufficient blinking;
- Advancing age is a risk factor for declines in tear production. Dry eye is more common in people age 50 years or older;
- Rosacea (an inflammatory skin disease) and blepharitis (an inflammatory eyelid disease) can disrupt the function of the Meibomian glands;
- Women are more likely to develop dry eye. Hormonal changes during pregnancy and after menopause have been linked with dry eye. Women also have an increased risk for autoimmune disorders;
- People in dry climates;
- People in dusty or smoky areas;
- Vitamin A deficiency are associated with dry eye;
- People who take certain medicines, such as:
- Anti-allergy medicines (antihistamine)
- Blood pressure medicines (antihypertensive)
- Birth control pills (oral contraceptive)
- Laxatives
- Tranquilisers.
SYMPTOMS
Symptoms in the eyes may include:
- Irritation;
- Itchiness;
- Redness;
- Burning;
- Inflammation of the eyelids;
- Feeling as though something is stuck in the eye;
- Light sensitivity;
- Increased sensitivity and discomfort when wearing contact lenses, if this applies;
- Vision that varies throughout the day;
- Occasional excessive tearing.
DIAGNOSIS
This condition is diagnosed based on your symptoms, your medical history, and an eye exam. Your health care provider may look at your eye using a microscope and may put dyes in your eye to check the health of the surface of your eye.
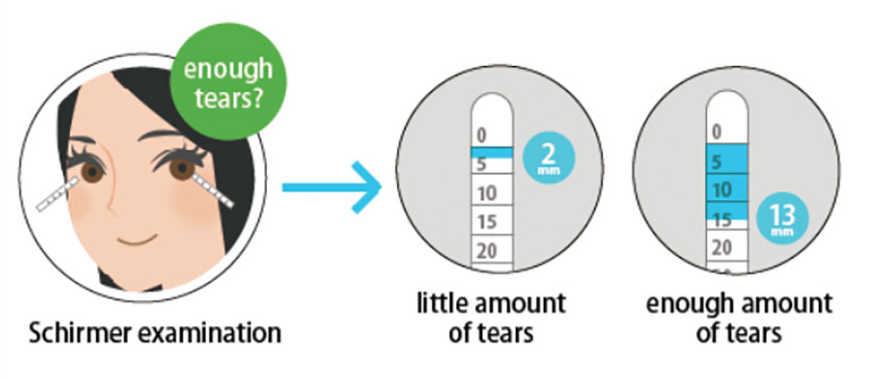
You may have to undergo a test to evaluate your tear production (Schirmer test). During this test, a small strip of special paper is gently pressed into the inner corner of your eye. Your tear production is measured by how much of the paper is moistened by your tears during a set amount of time.
TREATMENT
This condition is often treated at home. Your health care provider may recommend eye drops, which are also called artificial tears. If your condition is severe, treatment may include:
- Prescription eye drops
- Over-the-counter or prescription ointments to moisten your eyes
- Minor surgery to block tears from going into your nose
- Medicines to reduce inflammation of the eyelids.
HOME CARE INSTRUCTIONS
- Take, use, or apply over-the-counter and prescription medicines only as told by your health care provider. This includes eye drops.
- If directed, apply a warm compress to your eyes to help reduce inflammation. Place a towel over your eyes and gently press the warm compress over your eyes for about five minutes, or as long as told by your health care provider.
- If possible, avoid dry, drafty environments.
- Use a humidifier at home to increase moisture in the air.
- If you wear contact lenses, remove them regularly to give your eyes a break. Always remove contacts before sleeping.
- Keep all follow-up visits as told by your health care provider. This is important. This includes yearly eye exams and vision tests.
SEEK MEDICAL CARE IF:
- You have eye pain;
- You have pus-like fluid coming from your eye;
- Your symptoms get worse or do not improve with treatment.
SEEK IMMEDIATE MEDICAL CARE IF:
- Your vision suddenly changes.

 Vi
Vi