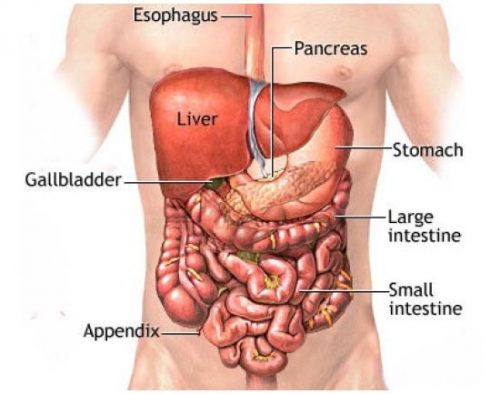
WHAT IS THE STOMACH?
The stomach is the digestive organ that is connected between the esophagus and the small intestine. Food enters the stomach through the esophagus where it is broken down and then transferred to the small intestine where the nutrients are absorbed.
WHAT IS GASTRECTOMY?
A gastrectomy is the surgical removal of all or part of the stomach. It is performed as treatment for stomach cancer, noncancerous tumors, gastric ulcers, a hole (perforation) in the stomach wall, or obesity.
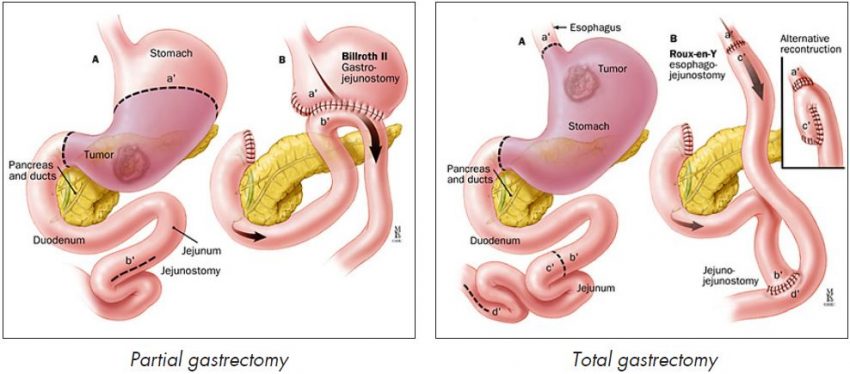
There are two main types of gastrectomy:
- A partial gastrectomy – where only part of the stomach is removed, and
- A total gastrectomy – where all of the stomach is removed.
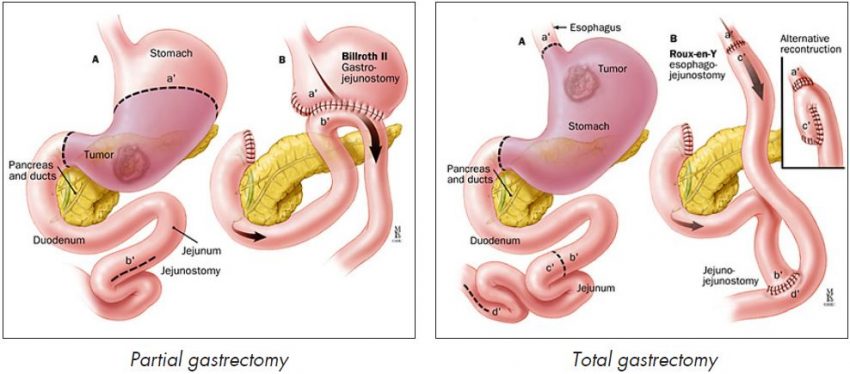
If you have a total gastrectomy, the surgeon will connect your oesophagus (the tube that runs from your throat to your stomach) to your bowel. This means that you will still have a working digestive system.
WHY IS IT NECESSARY?
Stomach cancer
A gastrectomy is one of the most effective ways to cure stomach cancer, or at least slow down the rate at which the condition spreads.
In most cases of stomach cancer, any tumours that are present will be too large to be cured using non-surgical methods, such as chemotherapy or radiotherapy (although these treatments are sometimes used to help make the surgery more successful). Therefore, it is necessary to remove some, or all, of the stomach and prevent cancerous cells spreading to other parts of the body.
If you have small tumours that are in the lower part of your stomach, you may only need to have a partial gastrectomy. However, if you have larger tumours that are in the middle or upper part of your stomach, it will probably be necessary to remove all of your stomach.
A gastrectomy may also be recommended if you develop a non-cancerous (benign) tumour in your stomach. Even though the tumour is not cancerous, there is a significant risk that it could eventually become cancerous if it is not removed.
Cancer of the oesophagus
A gastrectomy may also be required to treat cases of oesophageal cancer (cancer of the gullet) where it is thought that the cancer may have spread from the oesophagus to the top of the stomach.
Stomach ulcers
A gastrectomy used to be a common treatment for stomach ulcers (also known as peptic ulcers). However, medicines, such as proton pump inhibitors (PPIs), have been developed that are an effective and less invasive form of treatment.
A gastrectomy is only used to treat stomach ulcers in very rare cases where they fail to respond to other types of treatment.
Gastric perforation
Perforation can be caused by gastric ulcer or cancer, and gastrectomy is one option of treatment depends patient’s general condition, abdominal cavity, duration of disease…
Obesity
A type of gastrectomy, known as a vertical sleeve gastrectomy, can be used to treat people who are severely obese. Surgery involves removing up to 85% of the stomach, which means that the person is no longer able to eat large quantities of food, resulting in weight loss.
Vertical sleeve gastrectomy is sometimes used when people are too obese to safely undergo other types of obesity surgery, such as gastric banding or a gastric by-pass.
HOW IS IT PERFORMED?
Techniques used in gastrectomy
Gastrectomy is performed under general anesthesia.
There are two different techniques that can be used to carry out a partial or total gastrectomy. These are outlined below.
- Open gastrectomy – where the surgeon makes a large midline incision in your abdomen in order to remove some, or all, of your stomach.
- Laparoscopic or ‘keyhole’ gastrectomy – where the surgeon makes a number of smaller cuts in your abdomen, before using a special telescope and small surgical instruments to remove some, or all, of your stomach.
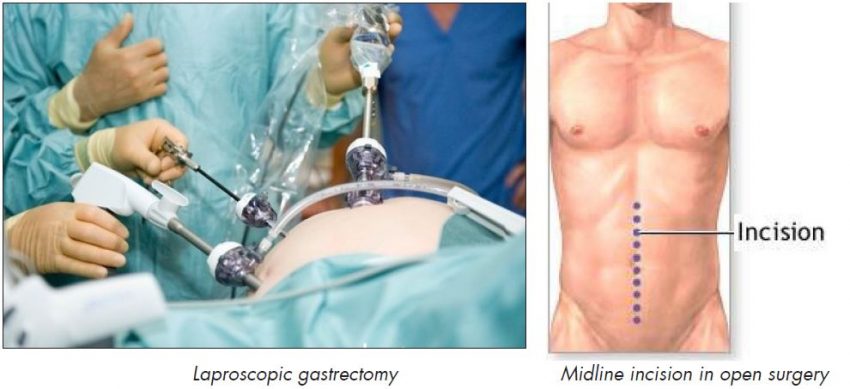
People who undergo a laparoscopic gastrectomy usually recover more quickly, and experience less pain following the procedure, than those who undergo an open gastrectomy.
However, open gastrectomies are usually more effective in treating advanced stomach cancer compared with laparoscopic gastrectomies.
Partial gastrectomy
The surgeon will remove the lower half of your stomach. Near-by lymph nodes are also usually removed because there could be a risk that the cancer has spread to the nodes.
Removing your lower stomach will expose your duodenum which is the first part of the small intestine. Your duodenum will be sown up and the upper part of your stomach will be moved down and reconnected to your small bowel.
Total gastrectomy
The surgeon will remove all of your stomach, then connect your oesophagus (the tube between your throat and stomach that food passes down) directly to your small bowel.
Vertical sleeve gastrectomy
The surgeon will remove the left side of your stomach. The remaining part of your stomach is resealed, using staplers, to create a much smaller and longer stomach that looks like a banana. This can reduce your stomach’s volume by up to 85%.
PREPARATION BEFORE OPERATION:
You will need to attend a pre-anesthesia appointment a few days before surgery. The appointment may involve having some blood tests and a general health check depending on your age and medical condition to make sure that you are fit for surgery.
It is recommended that you shower the night before and morning of the operation with Betadine scrub(an antiseptic solution).
After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon or anesthetist has told you are permissible to take with a sip of water the morning of surgery. If you have gastric outlet obstruction, you’ll need to have gastric lavage.
Risks of gastrectomy
Like any surgical procedure, a gastrectomy carries risks of complications. These complications may include pneumonia, urinary tract infection, heart attack…
For gastrectomies that are used to treat stomach cancer, the risk of complications is increased because the majority of people who have this type of surgery are elderly and often in a poor state of health.
Some possible surgical complications of gastrectomy include:
- Bleeding,
- Wound infection,
- Burst abdomen,
- Anastomotic leakage or duodenal stump leakage,
- Intra-abdominal abscess (a pus-filled swelling),
- Infection of the membrane that lines the abdominal cavity (peronitis),
- Anastomotic stenosis
Wound infection can usually be treated using antibiotics. Most other complications will require further surgery.
RECOVERY AFTER SURGERY
After the operation
Once you have had a gastrectomy operation, you will be fitted with a nasogastric tube, which is a thin tube that passes down your nose and into your stomach or small intestine. This allows the fluids that are produced by your stomach to be sucked out regularly without you feeling sick.
Until you are able to eat and drink normally, you will be fed intravenously (through a tube inserted directly into a vein). Most people are able to resume a light diet between 4-5 days after having a gastrectomy.
You will need to take painkillers for a few days. You should tell your treatment team if the painkillers that you are taking aren’t working because alternative painkillers are available.
Following a gastrectomy, you will probably be able to return home within 1-2 weeks after having the operation.
Adjusting to a new diet
Whatever type of gastrectomy you require, you will need to make changes to your diet. You may find that food or drink that you enjoyed before the operation, now gives you indigestion. Many people find that keeping a food diary enables them to record the effects that certain types of food have on their digestion.
It is likely that you will have to eat smaller, more frequent meals for quite a long time after having a gastrectomy. However, over time, your remaining stomach and/or small bowel will begin to stretch, and you will gradually be able to eat larger, less frequent meals.
You should avoid eating high-fibre foods immediately after having a gastrectomy because they will make you feel uncomfortably full. Over time, you will be able to gradually increase the amount of fibre in your diet.
Because one of your stomach’s functions is to absorb vitamins – particularly vitamin B12, vitamin C and vitamin D – from the food that you eat. You should eat foods that are high in calcium, iron, vitamin C, and vitamin D after gastrectomy.

 Vi
Vi 












