WHAT IS A LIVER RESECTION?
Liver resection, or hepatectomy, refers to the removal of a portion of the liver. This operation is usually done to remove various types of liver tumours, either primary (arisen within the liver) or secondary (spread to the liver from elsewhere). The principal aim of performing a liver resection is to completely remove the tumour without leaving any tumour behind.
WHERE IS THE LIVER AND WHAT ARE ITS FUNCTIONS?
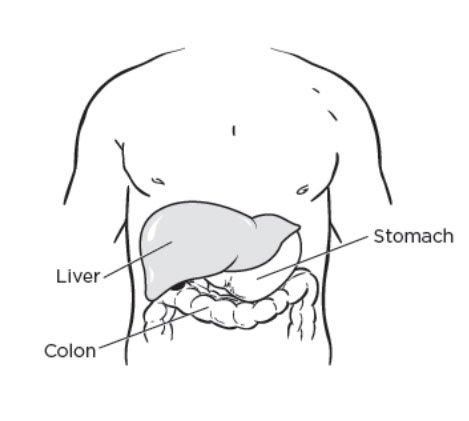
The liver is the largest solid organ in the body and is located in the upper right-quadrant of the abdomen under the rib cage. It is an important organ of the body without which we cannot survive.
Functionally, it is a major source of proteins for the body, processes much of the food we eat, is an important “filter” for the removal of drugs and toxins, and helps to fight infections. The liver also produces bile that is stored within the gallbladder and secreted via the bile ducts into the gut to facilitate absorption of fat.
The liver is the only organ in the body that has a double blood supply. Oxygenated blood flows in from the hepatic artery and nutrient rich blood flows through the portal vein from the gut. Blood leaves the liver through the 3 hepatic veins into the vena cava to return to the heart.
HOW IS THE LIVER DIVIDED UP?
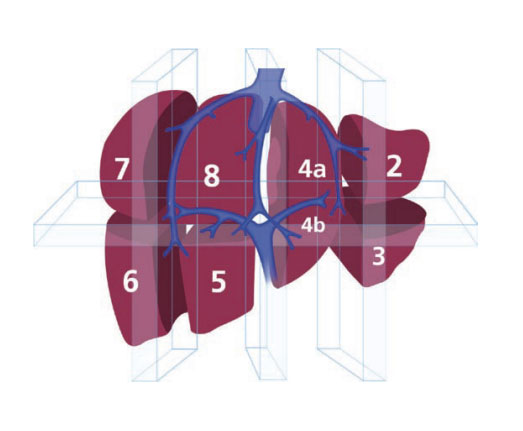
The liver can be divided into a right and left lobe. Within each lobe the liver can be divided into segments, based on the division of the blood vessels within the liver.
The extent of the liver resection depends on the size, number, and location of the tumour. The surgeon may remove a part of a segment (“wedge resection”), a segment, several segments, an entire lobe, or even a larger portion of the liver.
The liver has the ability to repair and regenerate (grow back) itself. Up to 65% of the liver can be removed. The remaining liver will regenerate itself following surgery and will grow back to its original size in about 3 months.
WHAT PATIENTS REQUIRE A LIVER RESECTION?
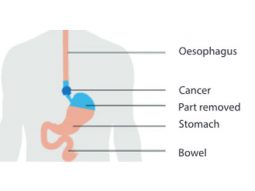
Most patients who require a liver resection have metastases (secondaries) from a colorectal (bowel) cancer. Less commonly, other secondary cancers from neuroendocrine tumours (like carcinoid), renal cancer or melanoma are resected.
The most common primary liver cancer that is resected is hepatocellular carcinoma (HCC or hepatoma). This is a cancer that originates in liver cells (primary), and is usually associated with underlying chronic liver disease. Primary cancers of the bile ducts, cholangiocarcinoma, are less commonly resected.
Whether this operation is a treatment option depends on:
- How much of the liver is affected;
- The size of the tumour(s);
- Where in the liver the tumours are located;
- Whether there are any tumours outside the liver;
- If you have a bowel cancer whether the tumour in your bowel has been treated or is treatable;
- Whether you have an underlying liver condition such as chronic hepatitis or cirrhosis and the extent of your liver dysfunction;
- Your general level of fitness.
Another indication for liver resection is liver stones (hepatolithiasis). The resection of the affected segment(s) of the liver removes stones, eliminates strictures and the consequent bile stasis which is responsible for stone formation, and eradicates the risk of cholangiocarcinoma
HOW IS A LIVER RESECTION PERFORMED?
The surgical procedure is performed under general anaesthesia and is quite lengthy, requiring between 3 and 6 hours, sometimes more. Most liver resections are performed during open surgery through an incision (cut) in your abdomen, called a laparotomy. However, sometimes the resection can be done through laparoscopy (minimally invasive surgery). This is not suitable for all patients for a number of reasons including the size and/or number of tumours to be removed. Laparoscopic resections are better tolerated with shorter hospital stay and less discomfort after the procedure.
WHAT CAN I EXPECT TO HAPPEN JUST AFTER THE OPERATION?
When your operation is finished you will be taken into the recovery room. When you are awake, you will be transferred to the Intensive Care Unit (ICU) where you will stay for 1 or 2 days, or until you are well enough to return to the ward.
In ICU, you will be attached to monitors that check your heart rate, blood pressure and fluid levels. You will be awake but it is quite normal to feel tired or sleepy.
WILL I BE IN PAIN AFTER THE OPERATION?
It is normal to have some pain after this type of operation. The anaesthetist and nurses will check to make sure that you are comfortable, and you will be given medication to keep you as pain free as possible. This is very important, as you will find it easier to breathe deeply, cough and move around. This will help reduce your risk of developing a chest infection and deep vein thrombosis.
After the procedure pain relief may be given using either an epidural that will stay in place for around 3 days after your operation or a parietal nerve block. You may also be connected to a special pump called a Patient-Controlled Analgesia pump (PCA) or have small tubes in your tummy giving local anaesthetic around your scar, called wound catheters. After the first 3 days, you will be given strong, pain relieving tablets.
If you are not comfortable, please tell the nurses looking after you so they can help.
ARE THERE ANY RISKS IN HAVING THE OPERATION?
There are risks with all surgery. Complications occur in about 20% of cases but most are mild and easily resolved.
Complications specific to undergoing liver resection include:
- Chest infection: because of the cut on your abdomen, you may find it difficult to breathe deeply or cough, which can lead to a chest infection. The physiotherapist and the nurses will teach you breathing exercises to help prevent a chest infection. We also encourage you to be up and mobile as soon as possible after your operation. The risk of respiratory complications is increased if you are overweight or if you smoke;
- Wound infection: despite antibiotic prophylaxis (antibiotics administered immediately before the procedure for a few hours, with a maximum duration of 24 hours) it happens that the wound can become infected. The nurses will check regularly for any signs of infection and keep the wound clean and dry. If an infection does develop you may be given antibiotics. Very occasionally, the wound may open and can then take a little bit longer to heal;
- Blood clots in the legs (deep vein thrombosis) and pulmonary embolism: moving around as soon as possible after your operation is recommended. We will give you special surgical stockings to wear whilst you are in hospital and injections to thin the blood. The physiotherapist will show you some leg exercises to help prevent blood clots, help you to stand and start walking slowly;
- Bile leak from the cut surface occurs in 5-10% of patients. This is usually self-limiting and is treated by external drainage. It may require an endoscopic procedure to decompress the bile ducts, and rarely reoperation is required;
- Bleeding either at the time of surgery or soon after may require blood transfusion or re-operation. In most instances it resolves without further intervention;
- Liver failure may occur if the liver remnant is insufficient to support normal function. This is more frequent in patients with chronic hepatitis and cirrhosis. Liver failure can lead to swelling of the legs, progressive jaundice (yellowing of the skin), and confusion. If this occurs you will be given medication to support your liver with medication until it recovers and liver medical specialists (hepatologists) will be involved in your care;
- Death: less than 1% of patients will die within 30 days after surgery due to serious complications associated with this operation or as a result of some other medical problem. You will be able to discuss your personal risks that apply to your surgery with the surgeon and anaesthetist prior to your operation. Because a liver resection is generally performed after a diagnosis of cancer, the risk of not having the surgery must be balanced against the risks of the surgery itself.
HOW LONG WILL I NEED TO STAY IN BED FOR?
Moving about as soon as possible after your operation will help to improve your circulation and prevent you from developing a chest infection, pneumonia and deep vein thrombosis. It will also help to stimulate your bowels to start working again.
For the first couple of days after the operation you will be attached to monitors and drips and you will feel tired and weak. A physiotherapist will teach you how to do deep breathing and leg exercises, and you will be encouraged to move around in your bed. You will be given help to get out of bed, sit in a chair and to walk a short distance as soon as possible after surgery.
HOW LONG WILL I BE IN HOSPITAL FOR?
Most patients are able to leave hospital 8 days after their operation. How long you are in hospital for will depend upon how quickly you recover from the operation, your general health and whether you develop any complications.
Once you are able to eat, drink and move about on your own, and your surgeon is satisfied with your progress and recovery you will be able to leave hospital.
WHEN CAN I GET BACK TO NORMAL?
It will be some time before you regain the energy you had before the operation. It is important to be aware that it may take many weeks and even some months before you feel completely fit again.
Rest as much as possible, gradually increasing your level of activity. It is important that you do some gentle exercise each day when you go home without over doing it. Gentle exercise such as walking and swimming will help you regain your strength.
You may need help with shopping and cleaning from family and friends for the first few weeks you are at home.
We advise that you avoid lifting heavy objects and driving for 6 weeks after your operation.
CAN I DRINK ALCOHOL AFTER GOING HOME?
It is wise to avoid any alcohol for at least 3 months after liver resection. This is the time when the liver will be regenerating. After this period you may take alcohol in moderation.

 Vi
Vi