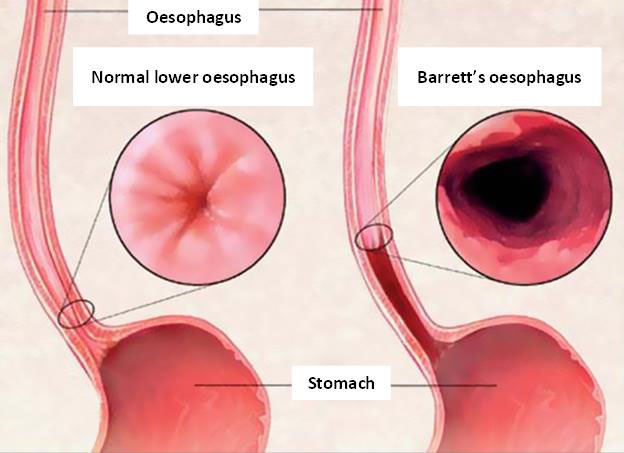
Barrett’s oesophagus, a condition in which the flat pink lining of the oesophagus is damaged by acid reflux, historically has received little attention but it’s important that its implications become more widely known.
People with chronic gastroesophageal reflux disease (GERD) have a higher risk of developing Barrett’s oesophagus, and those who have Barrett’s oesophagus have a higher risk of developing oesophageal cancer.

What is Barrett’s oesophagus?
Barrett’s oesophagus is a condition in which repeated exposure to acid reflux causes a change in the flat pink lining of the swallowing tube that connects the mouth to the stomach (the oesophagus). The cell layer of this lining becomes abnormal, thickening and turning red. If not treated promptly, the disease is likely to evolved into oesophageal cancer.
Symptoms of Barrett’s oesophagus
Barrett’s oesophagus may be asymptomatic or show acid reflux symptoms, including:
- Heartburn and regurgitation of stomach contents
- Difficulty swallowing food
- A burning sensation behind the sternum
- Vomiting after eating
Diagnosis of Barrett oesophagus
Advanced medical techniques and early diagnosis of Barrett’s oesophagus improves treatment efficacy and effectiveness:
- Gastroscopy: if the lower oesophageal lining changes in colour from normal pink to red, this indicates that Barrett’s oesophagus is progressing.
- Biopsy: If gastroscopy reveals signs of Barrett’s oesophagus, the doctor will take a few tissue samples from the oesophagus lining during endoscopy and send them to the lab for microscopic examination to confirm the diagnosis.
Is treatment for Barrett’s oesophagus effective?
Usually, the patient will be prescribed a change of lifestyle and a lifelong acid-inhibitor and periodic monitoring of their condition.
For patients with high-grade dysplasia or oesophageal cancer, surgery to remove the oesophagus may be necessary.
In addition to Barrett’s oesophagus treatments, which include photodynamic therapy, radiofrequency ablation and endoscopic mucosal resection, the application of Argon plasma has also been widely used and deemed a fast and highly effective approach. After receiving treatment via Argon plasma, the patient can be discharged from the hospital later the same day.
This technique utilises the energy of high-frequency electric current to discharge Argon at atmospheric pressure to coagulate tissue and destroys malignant cells irreversibly. The gastroenterologist can adjust the amperage to control the permeability of the Argon plasma, selectively destroy the diseased tissue and protect nearby healthy tissue, thereby increasing the accuracy and safety of this technique.
FV Hospital is the first medical centre in the South of Vietnam to apply Argon plasma technology to treat Barrett’s oesophagus, as well as to treat other gastrointestinal tract problems. FV Hospital is committed to always using the most advanced technologies and tools available to help improve treatment efficiency and safety for patients.
In addition, a safe, clean and sterile examination environment helps to minimise the risk of cross-contamination to help patients feel completely secure when visiting the hospital to receive care during the pandemic.

 Vi
Vi