Lung cancer, often termed a silent killer due to its quiet progression and high mortality risk. was the focus of the recent “Early Screening and Management of Early Lung Cancer” medical symposium hosted by FV Hospital in Ho Chi Minh City. Both local and international experts presented the latest advancements in early-stage lung cancer screening and treatment, highlighting the new opportunities for successful patient outcomes.


The “Early Screening and Management of Early Lung Cancer” medical symposium was chaired by Assoc. Prof Do Kim Que, MD, PhD – Vice Director of Thong Nhat Hospital, President of Asia Association of Thoracic and Cardiovascular Surgery, President of HCMC Association of Thoracic and Cardiovascular Surgery, and Vice President of Vietnam Association of Thoracic and Cardiovascular Surgery. Over 430 attendees, including doctors from Ho Chi Minh City and nearby provinces, gathered to hear prominent speakers from both domestic and international backgrounds share their expertise and practical insights on the diagnosis and treatment of lung cancer.

Assoc. Prof Do Kim Que, MD, PhD, emphasized the importance of the symposium: “This medical symposium is beneficial not only for doctors but also for nurses and patients, encouraging the community to engage in early screening and detection of lung cancer… We are very pleased that the symposium has brought together not only local doctors and speakers but also experts from France and Singapore, all sharing their experiences and knowledge in treating this leading cause of cancer-related deaths worldwide.”
Why does treating lung cancer remain a challenge?
In the opening presentation of the symposium, Dr Luong Ngoc Trung, MD, MSc – Head of Thoracic, Vascular and Endovascular Surgery Department at FV Hospital – stated that lung cancer is the most dangerous of all cancers. According to GLOBOCAN 2022 statistics, lung cancer ranks first among all cancer types, accounting for 12.4%, with the highest mortality rate at 18.7%.
Despite advances in medical science in cancer treatment overall, lung cancer remains a considerable challenge due to its very low 5-year survival rate (13-18%) and the lengthy, costly treatment process. This is largely because patients are often diagnosed at a late stage, where, after reaching stage 3A, surgery is usually no longer an option. “Among those diagnosed, only 25% of cases are eligible for surgery as a definitive treatment. This presents a significant burden for clinicians,” Dr Trung noted.
Therefore, early screening and detection are crucial. In the early stages, chances of a cure are significantly higher, the cost burden is reduced, and the 5-year survival prognosis for patients is greatly improved.
Advancements in Lung Cancer Screening
According to Dr Luong Ngoc Trung, there are now several methods for diagnosing lung cancer. Previously, doctors would use X-rays for lung cancer screening; however, this approach is no longer recommended, as it cannot detect small nodules around 5-6mm in size. Instead, patients are now advised to undergo a lung CT scan, which allows the detection of small lesions. This enables doctors to recommend further specialised tests to determine whether the growth is benign or malignant.

FV Hospital has implemented nearly all advanced techniques for early lung cancer screening and detection, including Low Dose CT Lung Cancer Screening, MRI, flexible bronchoscopy for cell sampling, transthoracic biopsy, and endobronchial ultrasound (EBUS) bronchoscopy. Additionally, the hospital utilises virtual navigation ultrasound technology, allowing doctors to perform bronchoscopy navigation that can be combined with EBUS for optimal results.
Another innovative technique, ICG (indocyanine green) dye marking, is also utilised at FV for detecting lesions in the lungs and gastrointestinal system. “This substance is injected into the patient’s bloodstream, and when it interacts with cancer cells, it changes colour, allowing surgeons to precisely remove lymph nodes and lung tumours, thereby reducing the chance of missing any high-risk nodules,” explained Dr Trung.
Dr Nguyen Van Tho, MD, PhD – Head of Department of Tuberculosis and Lung Diseases at the University of Medicine and Pharmacy, Ho Chi Minh City, also emphasised the importance of flexible bronchoscopy and endobronchial ultrasound (EBUS) in lung cancer diagnosis and staging. Flexible bronchoscopy enables doctors to examine the airways using a flexible tube with a small camera attached, enabling them to collect mucus or lung tissue samples for further analysis.
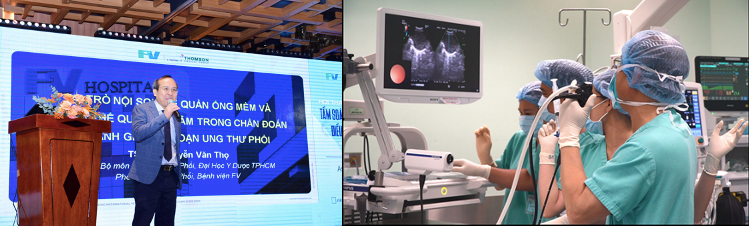
EBUS is a bronchoscopy technique combined with ultrasound, allowing observation and assessment of lesions in areas that traditional bronchoscopy methods may struggle to access. Additionally, the EBUS-TBNA (Endobronchial Ultrasound-guided Transbronchial Needle Aspiration) technique enables precise biopsy of mediastinal or hilar lymph nodes, which is essential for accurate lung cancer staging. The complication rate, including risks such as bleeding, pneumothorax, or infection, is as low as 1.23% – significantly lower than with previous techniques.
Dr Nguyen Van Tho, MD, PhD, noted that EBUS is now widely regarded as the “preferred technique” for biopsy and lung cancer diagnosis worldwide. In Vietnam, however, few hospitals have invested in this system due to its high cost and the substantial time required to train medical staff.
Lung cancer progresses silently and has become an increasingly complex disease in terms of identifying causative factors. Therefore, doctors recommend regular screening for those at risk. These include individuals who smoke regularly, those with a family history of lung cancer, patients with a history of exposure to radon, radiation, or uranium, and individuals aged between 50 and 80.
New treatment methods are expanding survival opportunities for lung cancer patients.
Currently, doctors have many “tools” to treat lung cancer, including surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. At the symposium, Dr Su Jang Wen, MBBS, MMed – Cardiothoracic Surgeon and Lung Cancer Specialist at the O2 Healthcare Group – shared his expertise in managing small nodules in the lungs, where cancer cells develop quietly.

Thanks to advancements in screening, it is now possible to detect very small nodules in the lungs ranging from 2-5mm, which were often overlooked in the past. Recent studies have shown that these small nodules can indicate early-stage lung cancer. When such nodules are detected, Dr Su advises patients to consider the option of surgery.
“A lung hospital in Shanghai found that 83% of lung nodules larger than 5mm developed into cancer. There is also an alarming rate of lung cancer cases in non-smokers. In fact, over 70% of lung cancer patients are diagnosed at an advanced stage. Early screening offers a much greater chance of saving lives,” Dr Su explained.

Over the past 15 years, Dr Su has successfully performed more than 7,000 lung surgeries using Video-Assisted Thoracic Surgery (VATS). This is a minimally invasive technique involving small incisions of only 1.5-3 cm. This approach results in fewer complications, minimal pain, and procedure times of around 30-35 minutes. Dr Su explained that over 98% of his patients in Singapore agree to undergo surgery for small lung nodules suspected of being cancerous. This is because, regardless of whether the biopsy results are benign or malignant, the surgery alleviates the patient’s anxiety, leading to better treatment outcomes.
In September 2024, FV Hospital officially partnered with Singapore’s O2 Healthcare Group to establish the FV Thoracic Surgery Centre. This centre offers diagnostic and surgical services for various thoracic diseases, including lung cancer, mediastinal tumours, oesophageal cancer, pneumothorax, chest wall conditions, and sympathectomy surgery. Vietnamese patients can now receive treatment from Dr Su Jang Wen and FV’s medical team without needing to travel abroad.
According to Dr Basma M’Barek, Head of Hy Vong Cancer Care Centre (Oncology Department) at FV Hospital, Stereotactic Body Radiation Therapy (SBRT) is a key treatment tool for lung cancer. When using radiation therapy on the lungs, it’s essential to consider tumour movement during breathing, as this can cause the radiation to be misdirected. At FV, doctors have incorporated a technique to actively synchronise with the patient’s breathing, helping to manage tumour movement. The SBRT method uses multiple radiation beams to deliver a high, focused dose of radiation with near-perfect precision to the targeted tissue, while rapidly reducing the dose to surrounding healthy tissues.

The advantage of SBRT over traditional radiation therapy is that it targets a smaller area, focusing directly on the tumour, minimising damage to lung tissue and reducing the radiation treatment time by 3-4 times, compared to the usual 6-7 sessions,” Dr Basma shared. She also emphasized the importance of cancer treatment units that integrate multiple specialties and establish Multidisciplinary Teams (MDT). Since 2003, FV Hospital has formed an MDT to evaluate each cancer case and create personalised treatment plans for each patient. “We meet weekly with surgeons, pathologists, radiologists, and other specialists to reach the optimal consensus for each cancer case,” Dr Basma added.

Ngoc Thach Hospital – shared his experience in diagnosing and treating non-small cell lung cancer. He explained that the diagnosis and treatment approaches at Pham Ngoc Thach Hospital, along with several other medical facilities in Vietnam, closely followed the recommendations of cancer associations and fully comply with the Ministry of Health’s treatment protocols. Given the range of treatment methods applicable at different stages, establishing Multidisciplinary Teams (MDTs) in hospitals is essential. “In reality, multidisciplinary consultations and multi-modality treatments, including surgery, chemotherapy, radiotherapy, targeted therapy, and immunotherapy help lung cancer patients extend their survival and improve their quality of life. However, doctors must always remember that the patient is at the centre of the treatment process, and we must consider their economic conditions and psychological well-being,” Dr Dung emphasised.

The “Early Screening and Management of Early Lung Cancer” symposium was highly regarded by attending doctors for its valuable and practical insights. The diagnostic techniques and advanced treatment methods presented by the speakers promise to open up new survival opportunities for many lung cancer patients.
| Lung Cancer Screening Programme at FV Hospital for only 2,570,000 VND The American Cancer Society recommends that individuals aged 55 to 74 with a long history of smoking (≥1 pack per day for 30 years or 2 packs per day for 15 years), or those who quit smoking within the past 15 years, should undergo annual screening with low-dose CT scans. This programme is also advised for individuals exposed to harmful environments such as tobacco smoke, asbestos, radon, arsenic, and other chemicals. If the results are normal, patients should continue with annual check-ups. If the results are abnormal, patients will be referred for consultation with a pulmonologist. Please contact: (028) 5411 3333. |

 Vi
Vi