After your amputation procedure, a wide range of healthcare professionals will be involved in your rehabilitation process:
- Your surgeons will start the rehabilitation process after surgery;
- Your nursing staff will take care of the wounds and give you advice on how to care for your stump;
- Your physiotherapists will help you recover your body functions and show you how to perform daily functional tasks;
- Your prosthetist will make and fit your prosthesis (artificial limb);
- Other professionals will assist you during your rehabilitation when required:
- General practice doctors will offer general care;
- Dieticians will provide necessary nutritional advice to promote healing and recovery, especially if you are diabetic;
- Clinical psychologists will support you in coping with the loss of your limb.
HOW WILL AMPUTATION AFFECT ME?
A lower limb amputation is a major traumatic event, affecting you both physically and mentally. It will change your life and create challenges in your day-to-day activities. You will experience things about which you may know very little and have little control over. You will most likely be frustrated at times and because the loss of a limb affects each person differently there is no simple answer – each amputee is an individual and faces their own unique challenges.
Fortunately, you do not have to figure it all out on your own. Whilst you and your situation are unique, there is a team of dedicated, experienced healthcare professionals ready to support and guide you through your rehabilitation.
HOW CAN REHABILITATION HELP ME RECOVER?
The rehabilitation team will work closely with you to improve your mobility and achieve functional independence in your day-to-day activities.
Your physiotherapist will advise you on progressive exercises designed to help the functional recovery of your stump, prepare you for wearing your prosthesis, recover a normal walking gait and learn how to live with your prosthesis., walk comfortably on stable or unstable surfaces, going up and downstairs, and become confident with your prosthesis.
Your prosthetist will also ensure that your prosthesis comfortably fits and adjust it when necessary, allowing you the best use of your prosthesis when walking returning to work and resuming your normal activities.

WHAT DOES THE REHABILITATION PROCESS INVOLVE?
After your surgery, your surgeon will refer you to the rehabilitation team so that you can start your rehabilitation without delay.
Your physiotherapist will advise you on daily exercise for your stump; on caring for your stump wound, scar and skin; on recovering the muscle and joint function in your residual leg as well as maintaining the functional capacity and strength of your other leg, arms and trunk. Initially, you may be advised to wear a compressive bandage to avoid swelling and maintain an appropriate stump shape.
When the scar on your stump is ready, your prosthetist will take a mould of your stump in order to make a preparatory prosthesis. This will take a few days. During this time, your physiotherapy will continue to improve your muscle function using apparatus like parallel bars, walking frame or crutches for gait training.
A first trial of your prosthesis will be arranged by the prosthetist and the physiotherapist. A few trials with adjustments will be required to achieve a comfortable fitting. Once this is achieved the rehabilitation team will deliver your prosthesis. As it heals your stump will shrink and change shape. socket adjustment, shank adjustment or additional layers of socks will be needed for the first few months to maintain comfort and effective functioning. During this period, do not hesitate to let your rehabilitation team know if you do not feel comfortable or your prosthesis does not feel right.
Remember, your rehabilitation team is ready to guide and support you, but you need to put in the work, follow their advice and let them know when, despite your best efforts, things just don’t seem to be working out for you.
Regular training with your prosthesis and gait training will be required until you feel completely confident in your daily life activities.
After around six months, your stump will not change any further, and your prosthetist will mould a new socket and fit you for a new prosthesis. This will be your definitive prosthesis.
HOW IS A PROSTHESIS DESIGNED?
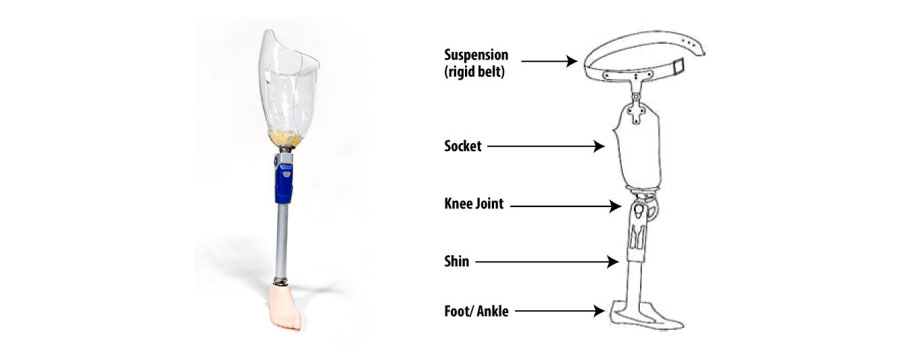
For aesthetic reasons, the shank on your definitive prosthesis will be covered by foam.
HOW DO I WEAR MY PROSTHESIS?
For complete contact between your stump and the prosthesis socket, stump “socks” are worn. These may be of different thicknesses and worn in layers. As your stump will continue to shrink down during the few first months, socks can be added in layers as needed.
Suspension (via a rigid belt) helps to keep your prosthesis in the correct place.
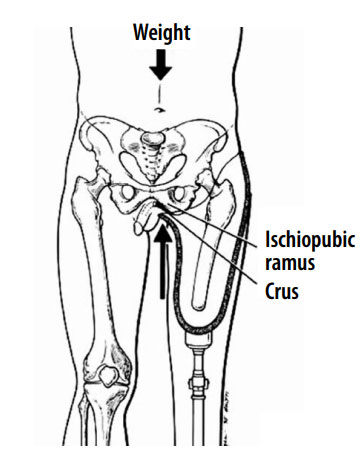
You should be able to balance and bear your weight well over both legs.
HOW DO I CARE FOR MY STUMP?
Your stump will be in contact with your prosthesis. Caring for your stump is essential.

- Check your skin daily for any broken areas. You may need to use a mirror or get someone else to check for you.
- Massage your stump as advised by your physiotherapist, particularly the scar and contact areas.
- Wash your stump twice a day with mild soap and warm water. If you are concerned about any scabs or unhealed areas, ask your doctor or nurses for advice.
- Always dry the skin thoroughly.
- If you experience any chafing or breakdown in the skin, stop using your prosthesis and seek advice from your rehabilitation team.
- Use clean socks daily, change as often as needed and wash them after wear.
- If you are a below-knee amputee, when not wearing your prosthesis keep your stump and your knee straight to prevent any stump swelling or joint contracture.
HOW DO I CARE FOR MY PROSTHESIS?
- Do not immerse your prosthesis in water.
- You can wipe the inside of the socket with a damp cloth. It’s a good idea to do this each night, giving the socket time to dry completely.
- The stocking covering the prosthesis can be cleaned with a damp cloth. If it gets very dirty, your prosthetist can change it for a new stocking.
- If you have any concerns regarding the mechanical state of your prosthesis, call the Physiotherapy & Rehabilitation Department immediately for advice.
HOW DO I CARE FOR MY REMAINING LEG?
Caring for your other leg is very important during your rehabilitation.
- Inspect your foot daily and seek medical advice if you have any cuts, blisters or inflamed areas.
- Wash your foot twice a day with soap and warm water.
- Always dry your foot thoroughly, especially between the toes.
- Avoid rubbing the skin too hard and forcing the toes apart.
- Cut your toenails and follow advice for treating corns or calluses.
- Use footwear that fits well and offers support and stability, with plenty of room for your toes and heel.
- Check your footwear regularly for rough edges or sharp areas.
HOW DO I USE MY PROSTHESIS AT HOME?
When your rehabilitation team is confident that you can use your prosthesis safely and independently, you will be able to take it home. That means you can increase the length of time you wear it during your normal everyday activities.
When in the rehabilitation room you will wear the prosthesis for up to two hours at a time, so when first taking it home you should wear it for one hour in the morning and one hour in the afternoon. Gradually increase the time of each of those sessions by half an hour until you can comfortably wear the prosthesis all day. Don’t expect to be walking all this time. Just do what you would do in the normal course of the day, seeing which functional tasks your prosthesis can help you to perform. Use assistive devices such as a walking frame or crutches as recommended by your physiotherapist.
HOW DO I DEAL WITH A PHANTOM LIMB?
A “phantom limb” is commonly experienced by amputees, often for an extended period. A phantom limb is the sensation that your amputated limb still there. If you have this sensation, be careful when you get up without your prosthesis – you could be at risk of falling!
HOW DO I DEAL WITH ANY PAIN?
Wound pain is often experienced after surgery. It is important to make your doctor aware of any pain you are experiencing so they can give you appropriate pain control. If the pain is well controlled you will be able to start exercising earlier and help your wound to heal.
Scar pain may be experienced. In this situation, tell your physiotherapist for arranging further pain management.
Along with the sensation of a phantom limb, some phantom pain can also occur. This is a form of nerve pain appearing from an area of the body that has been amputated. Many amputees experience phantom pain during the first three months of recovery, which may be severe or mild in nature. Phantom pain can interfere with your sleep and affect your general health and sense of wellbeing. Your physiotherapist can help you to manage this pain. Do not hesitate to ask for help.
WHAT ABOUT MY EMOTIONAL STATE?
You may experience an emotional sense of loss after your amputation procedure. You might feel sad, shocked or even angry. A period of bereavement is usually experienced and you might feel various emotions at different times as you face the challenge of readjusting. Talking about your feelings with your healthcare team can be very helpful.
WHAT KIND OF ASSISTANCE CAN I REQUEST DURING MY REHABILITATION?
After obtaining a medical referral, you can contact the Physiotherapy & Rehabilitation Department to book an appointment for any of the following services:
- Pain management for a phantom limb or joint pain
- Massage, exercising, stretching or strengthening
- Gait training during your rehabilitation progress
- Prosthesis trials
- Prosthesis adjustment or repair.
For advice on sporting activities, driving a car or motorbike or buying a wheelchair, contact your physiotherapist.
If you have any concerns about requesting a new prosthesis or regarding your current prosthesis, do not hesitate to contact the Physiotherapy & Rehabilitation Department for advice or to arrange an appointment.
FV Hospital, Physiotherapy & Rehabilitation Department, 1st floor
Tel (028) 54 11 33 40

 Vi
Vi 












