WHAT IS A TONSILLECTOMY?
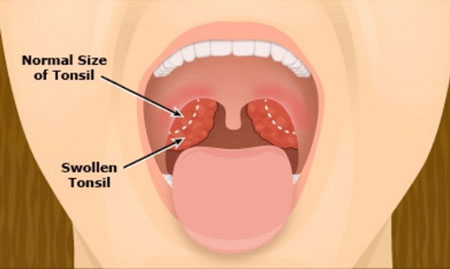
A tonsillectomy is the surgical removal of the tonsils. The tonsils are two small almond-shaped mounds of lymphatic tissue that sit on either side of the back of the throat. They are part of your body’s system to fight infection and are only important during the first few years of life. As we grow through childhood the tonsils usually shrink significantly.
This surgery is normally performed as a day case, which means you will come into hospital for the procedure and leave on the same day. It is performed under a general anaesthetic, which means you will be asleep for the entire operation.
Recovery time for a tonsillectomy is usually at least ten days to two weeks.
WHY IS IT DONE?
A tonsillectomy is used to treat:
- Recurring, chronic or severe tonsillitis
- Complications of enlarged tonsils
- Other rare diseases of the tonsils.
Tonsillitis
Tonsils produce certain types of disease-fighting white blood cells. Therefore, the tonsils act as the immune system’s first line of defence against bacteria and viruses that enter your mouth. This function may make them particularly vulnerable to infection and inflammation. The problem is more common in children because the immune system function of tonsils is most active before puberty. Also, unlike an adult’s immune system, a child’s system has had less exposure to bacteria and viruses and has yet to develop immunities to them.
A tonsillectomy may be recommended to prevent frequent, recurring episodes of tonsillitis.
Frequent is generally defined as:
- More than seven episodes a year
- More than five episodes a year in each of the preceding two years
- More than three episodes a year in each of the preceding three years.
The procedure may also be recommended if:
- A bacterial infection causing tonsillitis doesn’t improve with antibiotic treatment;
- An infection that results in a collection of pus behind a tonsil (tonsillar abscess) doesn’t improve with drug treatment or a drainage procedure.
Complications of enlarged tonsils
Tonsils may become enlarged after frequent or persistent infections, or they may be naturally large. A tonsillectomy may be used to treat the following problems caused or complicated by enlarged tonsils:
- Difficulty breathing
- Disrupted breathing during sleep
- Difficulty swallowing.
Other diseases of the tonsils
A tonsillectomy may also be used to treat other rare diseases or conditions of the tonsils, such as:
- Cancerous tissue in one or both tonsils
- Recurrent bleeding from blood vessels near the surface of the tonsils.
WHAT ARE THE RISKS OF HAVING A TONSILLECTOMY?
Tonsillectomy, like other surgeries, has certain risks:
- Reactions to anaesthetics: medication to make you sleep during surgery often causes minor, short-term problems, such as headache, nausea, vomiting or muscle soreness. The anaesthesiologist will explain the anaesthesia risks to you in more detail;
- Swelling: swelling of the tongue and soft roof of the mouth (soft palate) can cause breathing problems, particularly during the first few hours after the procedure;
- Bleeding during surgery: in rare cases, severe bleeding occurs during surgery and requires additional treatment and a longer hospital stay;
- Bleeding during healing: bleeding can occur during the healing process, up to two weeks after the operation;
- Infection: rarely, surgery can lead to an infection that requires further treatment.
HOW SHOULD YOU PREPARE?
You’ll receive instructions from the hospital on how to prepare yourself or your child for a tonsillectomy.
Information you’ll likely be asked to provide includes:
- All medications, including over-the-counter drugs and dietary supplements, taken regularly
- Personal or family history of adverse reactions to anaesthetics
- Personal or family history of bleeding disorders
- Known allergy or other negative reactions to medications, such as antibiotics.
Instructions for preparing will include the following:
- Don’t take aspirin or other medications containing aspirin for two weeks prior to surgery;
- Don’t eat or chew gum or drink milk or fruit juice with pulp for six hours before your surgery, but you can drink clear water, tea, coffee with or without sugar for up to two hours before your surgery;
- Do not smoke or drink alcohol for 24 hours prior to surgery;
- Make arrangements for a ride home;
- Plan for ten days to two weeks or more of recovery time. Adults may need more time than children do.
WHAT CAN YOU EXPECT?
Tonsillectomy is usually done as an outpatient procedure. That means you’ll be able to go home the day of the surgery. However, you will need to stay for six hours after your procedure so you can be observed for bleeding.
An overnight stay is possible if complications arise or if the surgery is done on a young child, or if you have a complex medical condition.
During the surgery
Because a tonsillectomy is performed under general anaesthesia, you or your child won’t be aware of the procedure or experience pain during the surgery.
The surgeon may cut out the tonsils using a blade (scalpel) or a specialised surgical tool that uses heat or high-energy heat (electro-cautery / diathermy dissection) to remove or destroy tissues and stop bleeding. Another technique is “coblation”, which stands for controlled ablation, it involves radiofrequency at a low temperature and uses a saline solution to gently and precisely remove the patient’s tonsils by destroying the surrounding tissues that attach them to the pharynx. Coblation is associated with less pain and a quicker return to normal diet and daily activity.
The procedure generally takes about 30 to 45 minutes.
During recovery
Two weeks off school or work after tonsillectomy are recommended.
Nearly everyone experiences pain after a tonsillectomy. You will have a sore throat when you wake up and this can last for a few days, and can also increase during the first few days. The pain can take up to 10-12 days to disappear completely. Some patients have an earache after the surgery. This is because the tonsils share some of the same nerves. This is normal and should go away in about two to three days.
Steps that you can take to reduce pain, promote recovery and prevent complications include the following:
- Medications: take pain medications as directed by your surgeon or the hospital staff;
- Fluids: it’s important to get plenty of fluids after surgery to avoid dehydration. Water and ice pops are good choices;
- Food: bland foods that are easy to swallow, such as applesauce or broth, are the best choices immediately after surgery. Foods such as ice cream and pudding can be added to the diet if they’re tolerated. Foods that are easy to chew and swallow should be added to the diet as soon as possible. Avoid acidic, spicy, hard or crunchy foods as they may cause pain or bleeding;
- Rest: bed rest is important for several days after surgery, and strenuous activities — such as running and bike riding — should be avoided for two weeks after surgery. You or your child should be able to return to work or school after resuming a normal diet, sleeping normally through the night and not needing pain medication. Talk to your doctor about any activities that should be avoided.
When to see the doctor or get emergency care
Watch for the following complications that require prompt medical care:
- Bleeding: you may see small specks of dark blood from the nose or in the saliva, but if you or your child coughs up, throws up, or spits out bright red blood or blood clots you must to come to the Accident and Emergency department for prompt evaluation and treatment. Although rare, this type of bleeding can occur up to two weeks after surgery. Surgery to stop bleeding may be necessary (about five out of 100 adults will return to hospital with bleeding which may need admission for observation or treating. Only one in a 100 will need to have a second operation to stop the bleeding);
- Fever: call your doctor if you or your child has a fever of 38°C or higher;
- Dehydration: call your doctor if you observe signs of dehydration, such as reduced urination, thirst, weakness, headache, dizziness or lightheadedness. Common signs of dehydration in children include sunken eyes, dry and sticky lips, no urine for over eight hours, and crying with no tears;
- Breathing problems: snoring or noisy breathing is common during the first week or so of recovery. However, if you or your child is having difficulty breathing, get emergency care.

 Vi
Vi