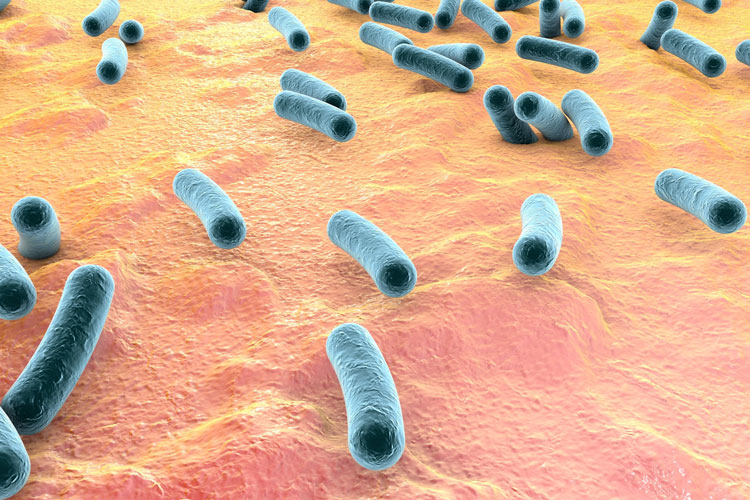
Tuberculosis is caused by a bacterium called Mycobacterium tuberculosis that spreads from person to person through microscopic droplets released into the air. This can happen when someone with the untreated, active form of tuberculosis coughs, speaks, sneezes, spits, laughs or sings.
Although tuberculosis is contagious, it’s not easy to catch. You are much more likely to get tuberculosis from someone you live with or work with than from a stranger. Most people with active TB who have had appropriate drug treatment for at least two weeks are no longer contagious.
LATENT TB INFECTION AND TB DISEASE
Not everyone infected with TB bacteria becomes sick. As a result, two TB-related conditions exist: latent TB infection and TB disease.
Latent TB Infection
TB bacteria can live in the body without making you sick. This is called latent TB infection. In most people who breathe in TB bacteria and become infected, the body is able to fight the bacteria to stop them from growing. People with latent TB infection do not feel sick and do not have any symptoms. People with latent TB infection are not infectious and cannot spread TB bacteria to others. However, if TB bacteria become active in the body and multiply, the person will go from having latent TB infection to being sick with TB disease.
TB Disease
TB bacteria become active if the immune system cannot stop them from growing. When TB bacteria are active (multiplying in your body), this is called TB disease. People with TB disease are sick. They may also be able to spread the bacteria to people they spend time with every day.
Many people who have latent TB infection never develop TB disease. Some people develop TB disease soon after becoming infected (within weeks) before their immune system can fight the TB bacteria. Other people may get sick years later when their immune system becomes weak for another reason.
For people whose immune systems are weak, especially those with HIV infection, the risk of developing TB disease is much higher than for people with normal immune systems.
TB DISEASE SYMPTOMS
Usually TB is revealed by fever, unexplained weight loss, drenching night sweats or a persistent cough.
Signs and symptoms of TB disease include:
- Coughing that lasts three or more weeks
- Coughing up blood
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue
- Fever
- Night sweats
- Chills
- Loss of appetite
Tuberculosis can also affect other parts of your body, including your kidneys, spine or brain. When TB occurs outside your lungs, signs and symptoms vary according to the organs involved. For example, tuberculosis of the spine may give you back pain, and tuberculosis in your kidneys might cause blood in your urine.
RISK FACTORS
Anyone can get tuberculosis, but certain factors can increase your risk of the disease. These factors include:
Weakened immune system
A healthy immune system often successfully fights TB bacteria, but your body cannot mount an effective defense if your resistance is low. A number of diseases and medications can weaken your immune system, including:
- HIV/AIDS
- Diabetes
- End-stage kidney disease
- Certain cancers
- Cancer treatment, such as chemotherapy
- Drugs to prevent rejection of transplanted organs
- Some drugs used to treat rheumatoid arthritis, Crohn’s disease and psoriasis
- Malnutrition
- Very young or advanced age
Traveling or living in certain areas
The risk of contracting tuberculosis is higher for people who live in or travel to countries that have high rates of tuberculosis and drug-resistant tuberculosis, such as:
- Sub-Saharan Africa
- India
- China
- Russia
- Pakistan
Poverty and substance abuse
- Lack of medical care.
- Substance abuse. IV drug use or alcohol abuse weakens your immune system and makes you more vulnerable to tuberculosis.
- Tobacco use. Using tobacco increases the risk of getting TB
Health care work
Regular contact with people who are ill increases your chances of exposure to TB bacteria. Wearing a mask and frequent hand-washing greatly reduce your risk
TESTING & DIAGNOSIS
1. Diagnosis of TB Disease
People suspected of having TB disease must have a medical evaluation, which will include:
- Medical history,
- Physical examination,
- Test for TB infection (TB skin test or TB blood test),
- Chest radiograph (X-ray), and
- Appropriate laboratory tests
Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has TB disease.
2. Tuberculin skin test
The TB skin test (also called the Mantoux tuberculin skin test) is performed by injecting a small amount of fluid (called tuberculin) into the skin in the lower part of the arm. A person given the tuberculin skin test must return within 48 to 72 hours to have a trained health care worker look for a reaction on the arm. The health care worker will look for a raised, hard area or swelling, and if present, measure its size using a ruler. Redness by itself is not considered part of the reaction.
The skin test result depends on the size of the raised, hard area or swelling. It also depends on the person’s risk of being infected with TB bacteria and the progression to TB disease if infected.
- Positive skin test: This means the person’s body was infected with TB bacteria. Additional tests are needed to determine if the person has latent TB infection or TB disease.
- Negative skin test: This means the person’s body did not react to the test, and that latent TB infection or TB disease is not likely.
3. TB blood tests
TB blood tests (also called interferon-gamma release assays or IGRAs) measure how the immune system reacts to the bacteria that cause TB. An IGRA measures how strong a person’s immune system reacts to TB bacteria by testing the person’s blood in a laboratory.
Two IGRAs are available:
– QuantiFERON®–TB Gold In-Tube test (QFT-GIT)
– T-SPOT®.TB test (T-Spot)
- Positive IGRA: This means that the person has been infected with TB bacteria. Additional tests are needed to determine if the person has latent TB infection or TB disease. A health care worker will then provide treatment as needed.
- Negative IGRA: This means that the person’s blood did not react to the test and that latent TB infection or TB disease is not likely.
IGRAs are the preferred method of TB infection testing for the following:
- People who have received Bacille Calmette–Guérin (BCG).
- People who have a difficult time returning for a second appointment to look for a reaction to the TST.
There is no problem with repeated IGRAs.
4. Imaging tests
If you have had a positive skin test, your doctor is likely to order a chest X-ray or a CT scan. This may show white spots in your lungs where your immune system has walled off TB bacteria, or it may reveal changes in your lungs caused by active tuberculosis. CT scans provide more-detailed images than do X-rays.
5. Sputum tests
If your chest X-ray shows signs of tuberculosis, your doctor may take samples of your sputum, which is the mucus that comes up when you cough. The samples are tested for TB bacteria.
Sputum samples can also be used to test for drug-resistant strains of TB. This helps your doctor choose the medications that are most likely to work. These tests can take four to eight weeks to be completed.

TREATMENT
1. Treatment for Latent TB Infection
People with latent TB infection are often prescribed treatment to prevent them from developing TB disease.
Because there are less bacteria in a person with latent TB infection, treatment is much easier. Four treatment regimens are approved for the treatment of latent TB infection. The medications used to treat latent TB infection include:
- isoniazid (INH)
- rifampin (RIF)
- rifapentine (RPT)
Certain groups of people (such as people with weakened immune systems) are at very high risk of developing TB disease once infected with TB bacteria. Every effort should be made to begin appropriate treatment and to ensure completion of the entire course of treatment for latent TB infection.
2. Treatment for TB Disease
TB disease can be treated by taking several drugs for 6 to 9 months. There are 10 drugs currently approved by the U.S. Food and Drug Administration (FDA) for treating TB. Of the approved drugs, the first-line anti-TB agents that form the core of treatment regimens include:
- Isoniazid (INH)
- Rifampin (RIF)
- Ethambutol (EMB)
- Pyrazinamide (PZA)
Regimens for treating TB disease have an initial phase of 2 months, followed by a choice of several options for the continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment).
The most common treatment protocol is:
- An initial 4-drug regimen for 2 months with isoniazid, rifampin, pyrazinamide, and ethambutol. Once the TB isolate is known to be fully susceptible, ethambutol can be discontinued.
- Then a 2-drug regimen for 4 months with isoniazid plus rifampin
It is very important that people who have TB disease finish the medicine, taking the drugs exactly as prescribed. If they stop taking the drugs too soon, they can become sick again; if they do not take the drugs correctly, the TB bacteria that are still alive may become resistant to those drugs. TB that is resistant to drugs is harder and more expensive to treat.
Patients with TB who are receiving pyrazinamide should undergo baseline and periodic serum uric acid assessments, and patients with TB who are receiving ethambutol therapy should undergo baseline and periodic visual acuity and red-green color perception testing.
TUBERCULOSIS: QUESTIONS AND ANSWERS
What is TB?
Tuberculosis (TB) is a disease caused by germs that are spread from person to person through the air. TB usually affects the lungs, but it can also affect other parts of the body, such as the brain, the kidneys, or the spine. A person with TB can die if they do not get treatment.
What are the Symptoms of TB?
The general symptoms of TB disease include feelings of sickness or weakness, weight loss, fever, and night sweats. The symptoms of TB disease of the lungs also include coughing, chest pain, and the coughing up of blood. Symptoms of TB disease in other parts of the body depend on the area affected.
How TB Spreads
TB is spread through the air from one person to another. The TB bacteria are put into the air when a person with TB disease of the lungs or throat coughs, sneezes, speaks, or sings. People nearby may breathe in these bacteria and become infected.
TB is NOT spread by:
- shaking someone’s hand
- sharing food or drink
- touching bed linens or toilet seats
- sharing toothbrushes
- kissing
What is the Difference between Latent TB Infection and TB Disease?
People with latent TB infection have TB germs in their bodies, but they are not sick because the germs are not active. These people do not have symptoms of TB disease, and they cannot spread the germs to others. However, they may develop TB disease in the future. They are often prescribed treatment to prevent them from developing TB disease.
People with TB disease are sick from TB germs that are active, meaning that they are multiplying and destroying tissue in their body. They usually have symptoms of TB disease. People with TB disease of the lungs or throat are capable of spreading germs to others. They are prescribed drugs that can treat TB disease.
What Should I Do If I Have Spent Time with Someone with Latent TB Infection?
A person with latent TB infection cannot spread germs to other people. You do not need to be tested if you have spent time with someone with latent TB infection. However, if you have spent time with someone with TB disease or someone with symptoms of TB, you should be tested.
What Should I Do if I Have Been Exposed to Someone with TB Disease?
People with TB disease are most likely to spread the germs to people they spend time with every day, such as family members or coworkers. If you have been around someone who has TB disease, you should go to your doctor for tests.
How Do You Get Tested for TB?
There are two tests that can be used to help detect TB infection: a skin test or TB blood test. The Mantoux tuberculin skin test is performed by injecting a small amount of fluid (called tuberculin) into the skin in the lower part of the arm. A person given the tuberculin skin test must return within 48 to 72 hours to have a trained health care worker look for a reaction on the arm. The TB blood tests measure how the patient’s immune system reacts to the germs that cause TB.
What Does a Positive Test for TB Infection Mean?
A positive test for TB infection only tells that a person has been infected with TB germs. It does not tell whether or not the person has progressed to TB disease. Other tests, such as a chest x-ray and a sample of sputum, are needed to see whether the person has TB disease.
What is Bacille Calmette–Guérin (BCG)?
BCG is a vaccine for TB disease. BCG is used in many countries. BCG vaccination does not completely prevent people from getting TB. It may also cause a false positive tuberculin skin test.
Why is Latent TB Infection Treated?
If you have latent TB infection but not TB disease, your doctor may want you to take a drug to kill the TB germs and prevent you from developing TB disease. The decision about taking treatment for latent infection will be based on your chances of developing TB disease. Some people are more likely than others to develop TB disease once they have TB infection. This includes people with HIV infection, people who were recently exposed to someone with TB disease, and people with certain medical conditions.
How is TB Disease Treated?
TB disease can be treated by taking several drugs for usually 6 months and for some cases up to 9 or even 12 months. It is very important that people who have TB disease finish the medicine, and take the drugs exactly as prescribed. If they stop taking the drugs too soon, they can become sick again; if they do not take the drugs correctly, the germs that are still alive may become resistant to those drugs. TB that is resistant to drugs is harder and more expensive to treat. In some situations, staff of the local health department meet regularly with patients who have TB to watch them take their medications. This is called directly observed therapy (DOT). DOT helps the patient complete treatment in the least
How can I keep from spreading TB?
The most important way to keep from spreading TB is to take all your medicines, exactly as directed by your doctor or nurse. You also need to keep all of your clinic appointments! Your doctor or nurse needs to see how you are doing. You may need another chest x-ray or a test of the phlegm you may cough up. These tests will show whether the medicines are working. They will also show whether you can still give TB bacteria to others. Be sure to tell the doctor about anything you think is wrong.
If you are sick enough with TB disease to go to a hospital, you may be put in a special room. These rooms use air vents that keep TB bacteria from spreading to other rooms. People who work in these special rooms must wear a special face mask to protect themselves from TB bacteria. You must stay in the room so that you will not spread TB bacteria to other people. Ask a nurse for anything you need that is not in your room.
If you are infectious while you are at home, there are things you can do to protect others near you:
- Take your medicines as directed. This is very important!
- Always cover your mouth with a tissue when you cough, sneeze, or laugh. Put the tissue in a closed bag and throw it away.
- Do not go to work or school. Separate yourself from others and avoid close contact with anyone. Sleep in a bedroom away from other family members.
- Air out your room often to the outside of the building (if it is not too cold outside). TB spreads in small closed spaces where air doesn’t move. Put a fan in your window to blow out (exhaust) air that may be filled with TB bacteria. If you open other windows in the room, the fan also will pull in fresh air. This will reduce the chances that TB bacteria will stay in the room and infect someone who breathes the air.
Remember, TB is spread through the air. People cannot get infected with TB bacteria through handshakes, sitting on toilet seats, or sharing dishes and utensils with someone who has TB.
After you take the medicines for about 2 or 3 weeks, you may no longer be able to spread TB bacteria to others. If your doctor or nurse agrees, you will be able to go back to your daily routine, including returning to work or school. Remember, you will get well only if you take your medicines exactly as directed by your doctor or nurse.
Think about people who may have spent time with you, such as family members, close friends, and coworkers. The local health department may need to test them for TB infection. TB is especially dangerous for children and people infected with HIV. If infected with TB bacteria, these people need medicine right away to keep from developing TB disease

What are the side effects of TB disease medicines?
If you are taking medicines for TB disease, you should take it as directed by your doctor or nurse. The medicines may cause side effects. Some side effects are minor problems. Others are more serious. If you have a serious side effect, call your doctor or nurse immediately. You may be told to stop taking your medicine or to return to the clinic for tests.
The side effects listed below are serious. If you have any of these symptoms, call your doctor or nurse immediately:
- No appetite
- Nausea
- Vomiting
- Yellowish skin or eyes
- Fever for 3 or more days
- Abdominal pain
- Tingling in the fingers or toes
- Pain in the lower chest or heart burn
- Feeling itchy
- Skin rash
- Easy bruising
- Bleeding from gums
- Nose bleeding
- Urine becomes dark or brown in color
- Aching joints
- Dizziness
- Tingling or numbness around the mouth
- Blurred or changed vision
- Ringing in the ears
- Hearing loss
The side effects listed below are minor problems. If you have any of these side effects, you can continue taking your medicine:
- Rifampin can turn urine, saliva, or tears orange. The doctor or nurse may advise you not to wear soft contact lenses because they may get stained.
- Rifampin can make you more sensitive to the sun. This means you should use a good sunscreen and cover exposed areas so you don’t burn.
- Rifampin makes birth control pills and implants less effective. Women who take rifampin should use another form of birth control.
- If you are taking rifampin as well as methadone (used to treat drug addiction), you may have withdrawal symptoms. Your doctor or nurse may need to adjust your methadone dosage.
Add if you want more information please contact the department of internal medicine….

 Vi
Vi