What are varicose veins?
Arteries bring oxygen-rich blood from your heart to the rest of your body and veins return oxygen-poor blood back to your heart.
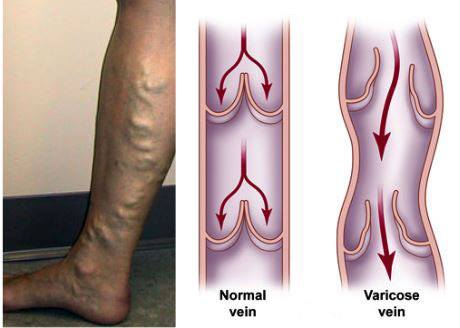
Varicose veins are swollen veins that you can see through your skin. They often look blue, bulging, and twisted. Left untreated, varicose veins may worsen over time. Varicose veins can cause aching and feelings of fatigue as well as skin changes like rashes, redness, and sores.
You have three kinds of veins in your legs; the superficial veins, which lie closest to your skin, the deep veins, which lie in groups of muscles and perforating veins, which connect the superficial veins to the deep veins. The deep veins lead to the vena cava, your body’s largest vein, which runs directly to your heart. Varicose veins occur in the superficial veins in your legs.
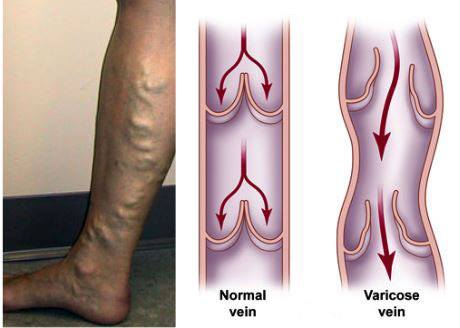
When you are in the upright position, the blood in your leg veins must work against gravity to return to your heart. To accomplish this, your leg muscles squeeze the deep veins of your legs and feet. One-way flaps, called valves, in your veins keep blood flowing in the right direction. When your leg muscles contract, the valves inside your veins open. When your legs relax, the valves close. This prevents blood from flowing in reverse, back down the legs. The entire process of sending blood back to the heart is called the venous pump.
When you walk and your leg muscles squeeze, the venous pump works well. But when you sit or stand, especially for a long time, the blood in your leg veins can pool and the pressure in your veins can increase. Deep veins and perforating veins are usually able to withstand short periods of increased pressures. However, if you are a susceptible individual, your veins can stretch if you repeatedly sit or stand for a long time. This stretching can sometimes weaken the walls of your veins and damage your vein valves. Varicose veins may result.
What are the symptoms?
If you have varicose veins, your legs may feel heavy, tired, restless, or achy. Standing or sitting for too long may worsen your symptoms. You may also experience night cramps.
You may notice small clusters of veins in a winding pattern on your leg, or soft, slightly tender knots of veins. Sometimes, the skin on your legs may change colour, become irritated, or even form sores.
If you have severe varicose veins, you have slightly increased chances of developing Deep Vein Thrombosis (DVT). DVT may cause sudden, severe leg swelling. DVT is a serious condition that requires immediate medical attention.
What causes varicose veins?
High blood pressure inside your superficial leg veins causes varicose veins.
Factors that can increase your risk for varicose veins include having a family history of varicose veins, being overweight, not exercising enough, smoking, standing or sitting for long periods of time, or having DVT. Women are more likely than men to develop varicose veins. Varicose veins usually affect people between the ages of 30 and 70.
Pregnant women have an increased risk of developing varicose veins, but the veins often return to normal within one year after childbirth. Women who have multiple pregnancies may develop permanent varicose veins.
What tests will I need?
First, your doctor will ask you questions about your general health, medical history, and symptoms and will conduct a physical exam. Your doctor will examine the texture and colour of any prominent veins. He or she may apply a tourniquet or direct hand pressure to observe how your veins fill with blood. To confirm a diagnosis of varicose veins, your doctor may order a duplex ultrasound test.
Duplex ultrasound uses painless, high-frequency waves higher than human hearing can detect. Your doctor uses duplex ultrasound to measure the speed of blood flow and to see the structure of your leg veins. The test can take approximately 20 minutes for each leg. Besides showing varicose veins, duplex ultrasound may help your doctor decide whether your varicose veins could be related to some other condition rather than the veins themselves.
How are varicose veins treated?
Varicose veins may sometimes worsen without treatment. Your doctor will first try methods that don’t require surgery to relieve your symptoms. If you have mild to moderate varicose veins, elevating your legs can help reduce leg swelling and relieve other symptoms. Your doctor may instruct you to prop your feet up above the level of your heart three or four times a day for about 15 minutes at a time.
When you need to stand for a long period of time, you can flex your legs occasionally to allow the venous pump to keep blood moving toward your heart.
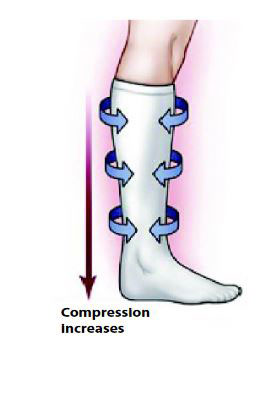
Compression stockings
For more severe varicose veins, your doctor may prescribe compression stockings. Compression stockings are elastic stockings that squeeze your veins and stop excess blood from flowing backward. In this way, compression stockings also can help heal skin sores and prevent them from returning. You may be required to wear compression stockings daily for the rest of your life. For many patients, compression stockings effectively treat varicose veins and may be all that are needed to relieve pain and swelling and prevent future problems.
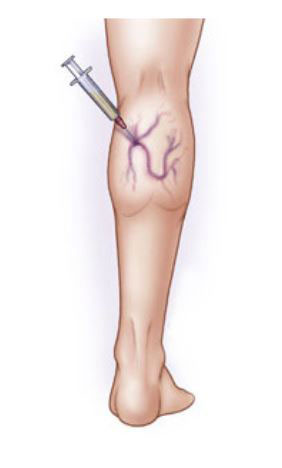
Sclerotherapy
During sclerotherapy, your doctor injects a chemical into your varicose veins. The chemical irritates and scars your veins from the inside out so your abnormal veins can then no longer fill with blood. Blood that would normally return to the heart through these veins returns to the heart through other veins. Your body will eventually absorb the veins that received the injection.
Since radiofrequency and laser treatments have been introduced sclerotherapy is now rarely performed.
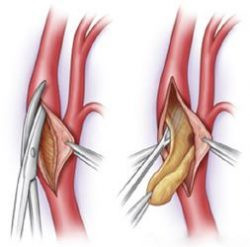
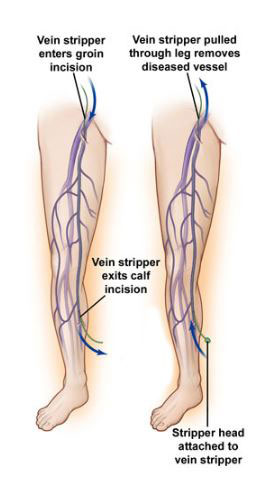
Vein stripping
To perform vein stripping, your doctor first makes a small incision in the groin area and usually another incision in your calf below the knee. Then your doctor disconnects and ties off all major varicose vein branches associated with the saphenous vein, the main superficial vein in your leg. Your doctor then removes the saphenous vein from your leg.
This procedure is nowadays reserved to the few cases for which radiofrequency or laser treatment are not recommended.
Endovenous ablation of varicose veins by laser or radiofrequency
Endovenous ablation is an image-guided, minimally invasive, thermal treatment that uses radiofrequency or laser energy to cauterise (burn) and close varicose veins. Thermal ablation is safe, less invasive than surgery, and leaves virtually no scars.
The doctor uses ultrasound to visualise the vein. Using ultrasound guidance, the doctor inserts a catheter through a small incision and positions it within the abnormal vein. A laser fibre or a radiofrequency electrode (both are long thin wires that carry energy from power generators) is inserted through the catheter and moved to the desired location within the vein. Local anaesthesia is injected into the tissues around the vein to collapse the vein around the fibre or electrode and act as insulation for the energy’s heat. The energy heats the vessel and causes it to close. Following the procedure, the faulty vein will shrink and “scar down.”
This procedure is usually done on an outpatient basis.
Some post-procedure bruising and tenderness may occur. Wearing a compression stocking for two weeks is recommended to ease these side effects.
Venous ablation using VenaSealTM closure system
This is a new, non-thermal, technique using a cyanoacrylate glue (medical adhesive) to occlude varicose veins.
During the procedure, the doctor fills a syringe with the medical adhesive, and inserts it into the VenaSeal™ closure system’s dispensing gun that is attached to a catheter. The catheter is advanced into the diseased vein under ultrasound guidance. The catheter is placed in specific areas along the diseased vein then the doctor conducts a series of trigger pulls to deliver the medical adhesive. Compression is applied to the leg during the procedure.
This procedure is designed to minimise patient discomfort and reduce recovery time. After the procedure, a small bandage will be placed at the access site. Patients are able to rapidly return to normal activities. This treatment has been shown to be effective with demonstrated safety and high closure rates.
Laser treatment of spider veins
Spider veins, or telangiectasias, are those small red, blue and purple blood vessels that appears most frequently on face and thigh. They are in reality small varicose veins.
Laser treatment is the best choice for spider veins. Light energy is delivered through a special hand-piece to the targeted veins, in a series of brief pulses, generating heats that destroy the blood vessels but not the surrounding tissues.
Most veins will disappear in two to six weeks. Hot baths and strenuous exercise should be avoided for a few weeks, as well as exposure to sunlight.

Living with varicose veins
Varicose and spider veins might not always require medical treatment. If varicose veins make walking or standing painful, you should talk to your doctor for advice. You should also see your doctor if a sore develops on or near a varicose vein, or if your feet or ankles swell.
In some cases, varicose veins can be harmful to your health because they might be associated with the development of:
- Venous stasis ulcers: these ulcers result when the enlarged vein does not provide enough drainage of fluid from the skin. The skin does not receive enough oxygen and an ulcer (skin sore) might form;
- Phlebitis: Inflammation of the vein;
- Thrombosis: development of blood clots that form in the dilated vein.
Lifestyle and home remedies
There are some self-care measures you can take to decrease the discomfort that varicose veins can cause. These same measures can help prevent or slow the development of varicose veins, as well. They include:
- Exercise: get moving. Walking is a great way to encourage blood circulation in your legs. Your doctor can recommend an appropriate activity level for you;
- Watch your weight and your diet: shedding excess pounds takes unnecessary pressure off your veins. What you eat can help, too. Follow a low-salt diet to prevent swelling caused from water retention;
- Watch what you wear: avoid high heels. Low-heeled shoes work calf muscles more, which is better for your veins. Don’t wear tight clothes around your waist, legs or groin because these garments can reduce blood flow;
- Elevate your legs: to improve the circulation in your legs, take several short breaks daily to elevate your legs above the level of your heart. For example, lie down with your legs resting on three or four pillows;
- Avoid long periods of sitting or standing: make a point of changing your position frequently to encourage blood flow.

 Vi
Vi