Sometimes, an epidural may not work. This can happen if:
- It’s difficult to find the epidural space
- The local anaesthetic doesn’t spread evenly around the epidural space
- The catheter falls out
If your epidural doesn’t work, your anaesthetist may offer alternative pain relief or perform the procedure again. Epidural anaesthesia is usually safe; however, as with most medical procedures, side effects can sometimes occur.
LOW BLOOD PRESSURE
Low blood pressure (hypotension) is the most common side effect associated with having an epidural. This is because the local anaesthetic used affects the nerves that go to your blood vessels, leading to a fall in blood pressure. This may cause nausea, dizziness and lightheadedness (a feeling as if you might faint, your body may feel heavy while your head feels as if it is not getting enough blood)
Your blood pressure will be closely monitored while you’re having an epidural. If necessary, medication can be passed through a drip to treat low blood pressure.
LOSS OF BLADDER CONTROL
After having an epidural, you will not be able to feel when your bladder is full because the epidural affects the surrounding nerves.
A catheter inserted into your bladder allows urine to drain away. Your bladder control will return to normal as soon as the epidural wears off.
ITCHY SKIN
Sometimes, the painkillers combined with the anaesthetic during an epidural can cause itchiness. This can usually be easily treated.
SICKNESS
You may feel sick (or be sick) after having an epidural. If your blood pressure is normal, anti-sickness medicines will usually help.
BACKACHE
A study carried out in 2010 found no increased risk associated with the use of epidural anaesthesia and long-term backache.
Your epidural care team will try to make sure you’re comfortable during and after the procedure, but being in the same position for a long time may make existing backache worse.
If you experience severe backache following an epidural, you should let your care team know as soon as possible, so they can investigate the problem.
SEVERE HEADACHE
Occasionally, a severe headache can develop after an epidural – known as a post-dural puncture headache.
This happens when the lining of your spinal cord (dura) is accidentally punctured.
The headache usually clears up with time, but a procedure known as a “blood patch” may be used to seal up the hole. It involves taking a small sample of your blood and injecting it into the epidural space. When the blood clots (thickens), the hole will be sealed and your headache will stop.
Headaches caused by a punctured dura are rare following an epidural. There’s a 1 in 100 to 1 in 500 chance of it happening.
INFECTION
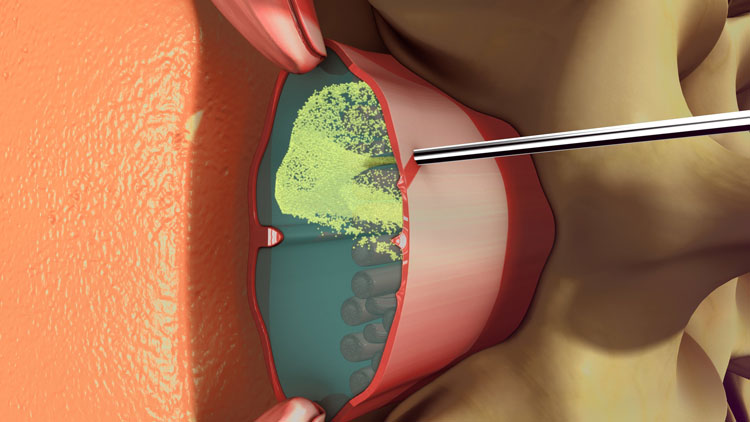
It’s possible for an infection to develop at the site of the injection in the weeks following an epidural. This can lead to an abscess forming. Very rarely, abscesses can form in the epidural space. This may lead to nerve damage, including the complete loss of movement of the lower half of the body (paraplegia).
EPIDURAL HAEMATOMA
An epidural haematoma is a very rare complication of an epidural. A haematoma is a collection of blood that develops as a result of a break in a blood vessel wall.
If the veins inside the epidural space are punctured, blood can build up and a haematoma can develop, causing pressure on your spinal cord.
Very rarely, this may lead to nerve damage, such as paraplegia.
OTHER COMPLICATIONS
Other possible, although rare, complications of an epidural include:
- Fits (convulsions)
- Breathing difficulties
- Nerve damage
- Death
However, serious complications following an epidural are rare. The best estimate of the overall risk of permanent harm from an epidural in labour is between 1 in 80,000 and 1 in 320,000.
Before deciding to have an epidural, you should discuss the procedure with your anaesthetist. They can provide further information and advice on the risks of developing complications such as those described above.

 Vi
Vi 












